Excretory System
Article objectives
If you exercise on a hot day, you are likely to lose a lot of water in sweat. Then, for the next several hours, you may notice that you do not pass urine as often as normal and that your urine is darker than usual. Do you know why this happens? Your body is low on water and trying to reduce the amount of water lost in urine. How does the body know when it is low on water? How does it control the amount of water lost in urine? The answers to both questions are the kidneys and the glands that control them.
Homeostasis and Excretion
The kidneys are the body’s main organs of homeostasis and excretion. Homeostasis is the body’s attempt to maintain a constant internal environment. One of the major ways the body achieves homeostasis is through excretion. Excretion is the process of removing wastes and excess water from the body.
Homeostasis
Homeostasis is a fundamental characteristic of all living things. Internal body conditions must be kept within certain limits for the normal functioning of cells. Homeostasis involves keeping many internal factors at more or less constant levels. The factors include body temperature and properties of the blood. For example, the blood must have certain levels of acidity, salts, and nutrients in order for cells to function normally.
A variety of homeostatic mechanisms help maintain stability of the internal environment. Each mechanism involves the interaction of at last three components: a receptor, a control center, and an effector.
• The receptor senses changes in the internal environment and sends the information to the control center.
• The control center processes the information, determines the appropriate action, and sends a command to the effector.
• The effector responds to the command and changes conditions in the internal environment.
An example of a homeostatic mechanism in humans is the regulation of body temperature. This is represented by the diagram in Figure 1. Temperature receptors in the skin send information about skin temperature to the brain. The brain is the control center. It determines whether the temperature is too high or too low and sends appropriate commands to effectors that control body temperature. Effectors include blood vessels near the surface of the body. If the temperature is too high, the brain commands the blood vessels to dilate, which helps the body lose heat. If the temperature is too low, the brain commands the blood vessels to constrict, which helps the body retain heat. These actions help return body temperature to normal.

Figure 1: Regulation of body temperature is an example of negative feedback. When body temperature deviates from normal, this information feeds back to the brain and sets in motion changes that return body temperature to normal.
Negative Feedback and Body Temperature
The regulation of body temperature is an example of negative feedback. Negative feedback is a type of homeostatic mechanism in which change in one direction results in a counteractive change in the opposite direction. Negative feedback reverses the direction of change to bring conditions back to normal. Most of the mechanisms that control homeostasis in the human body involve negative feedback.
Positive feedback mechanisms also exist, but they are not common in the human body. Positive feedback accelerates or amplifies a change and pushes levels farther away from normal. One example of a positive feedback mechanism in the body is blood clotting.
If homeostasis is disturbed, a homeostatic imbalance results. This may result in cells getting too much or not enough of certain substances. Many diseases are caused by homeostatic imbalances. For example, diabetes mellitus is a disease in which the blood contains too much glucose. This can have serious consequences for cells throughout the body. It may lead to damaged blood vessels, heart disease, blindness, and kidney failure.
Excretion
Excretion is an essential process in all forms of life. When cells metabolize—or break down—nutrients, waste products are produced. For example, when cells metabolize proteins and nucleic acids, nitrogen wastes such as ammonia, urea and uric acid are produced. Ammonia is a toxic substance and must be removed from the blood and excreted from the body. Urea is removed through urine, which is produced in the kidney. Excretion is also necessary to remove excess water, salts, and many other substances from the body. Although the kidneys are the main organs of excretion of wastes from the blood, several other organs are also involved in excretion, including the large intestine, liver, skin, and lungs.
• The large intestine eliminates solid wastes that remain after the digestion of food in the gastrointestinal tract.
• The liver breaks down excess amino acids in the blood to form ammonia, and then converts the ammonia to urea, a less toxic substance. The liver also breaks down other toxic substances in the blood, including alcohol and drugs.
• The skin eliminates water and salts in sweat.
• The lungs exhale water vapor and carbon dioxide.
Kidneys and Excretion
The kidneys are part of the urinary system. The kidneys work together with other urinary system organs in the function of excretion. The urinary system is shown in Figure 2.

Figure 2: The urinary system.
Urinary System
In addition to the kidneys, the urinary system includes the ureters, bladder, and urethra. The main function of the urinary system is to filter waste products and excess water from the blood and remove them from the body. The two kidneys, which are described in detail below, filter the blood and form urine. Urine is the liquid waste product of the body that is excreted by the urinary system.
From the kidneys, urine enters the ureters, which carry it to the bladder. Each ureter is a muscular tube about 25 centimeters long. Peristaltic movements of the muscles of the ureter send urine to the bladder in small spurts.
The bladder is a hollow organ that stores urine. It can stretch to hold up to 500 milliliters. When the bladder is about half full, the stretching of the bladder sends a nerve impulse to the sphincter that controls the opening to the urethra. In response to the impulse, the sphincter relaxes and lets urine flow into the urethra.
The urethra is a muscular tube that carries urine out of the body. Urine leaves the body through another sphincter in the process of urination. This sphincter and the process of urination are normally under conscious control.
Kidneys
The kidneys participate in whole-body homeostasis. As mentioned above, one of the promary roles of the kidney is to remove nitrogenous wastes. The kidneys are a pair of bean-shaped, reddish brown organs about the size of a fist. They are located just above the waist at the back of the abdominal cavity, on either side of the spine. As shown in Figure 2, the kidneys are protected by the ribcage. They are also protected by a covering of tough connective tissues and two layers of fat, which help cushion them.
Located on top of each kidney is an adrenal gland, also shown in Figure 2. The two adrenal glands secrete several hormones. Hormones are chemical messengers in the body that regulate many body functions. The adrenal hormone aldosterone helps regulate kidney functions.

Figure 3: The human kidney.
In Figure 3, you can see that the kidney has three layers. The outer layer is the renal cortex, and the middle layer is the renal medulla. The inner layer, the renal pelvis, is where the renal artery enters the kidney and the renal vein exits the kidney. The renal artery carries blood to the kidney to be filtered, and the renal vein carries the filtered blood away from the kidney. Structures in the kidney called nephrons are also seen in Figure 3. Each nephron extends from the cortex down into the medulla.
Nephrons
Nephrons are the structural and functional units of the kidneys. A single kidney may have more than a million nephrons. The diagram in Figure 4 represents an individual nephron and shows its main structures and functions. The structures include the glomerulus, Bowman’s capsule, and renal tubule.

Figure 4: Nephron structures and functions.
• The glomerulus is a cluster of arteries that filters substances out of the blood.
• Bowman’s capsule is a cup-shaped structure around the glomerulus that collects the filtered substances.
• The renal tubule is a long, narrow tube surrounded by capillaries that reabsorbs many of the filtered substances and secretes other substances.
Filtration, Reabsorption, and Secretion
The renal arteries, which carry blood into the kidneys, branch into the capillaries of the glomerulus of each nephron. The pressure of blood moving through these capillaries forces some of the water and dissolved substances in the blood through the capillary walls and into Bowman’s capsule. Bowman’s capsule is composed of layers. The space between the layers, called Bowman’s space, fills with the filtered substances.
The process of filtering substances from blood in the glomerulus is called filtration. The fluid that collects in Bowman’s space is called filtrate. It is composed of water, salts, glucose, amino acids, and urea. Larger structures in the blood—including protein molecules, blood cells, and platelets—do not pass into Bowman’s space. Instead, they return to the main circulation.
From Bowman’s space, the filtrate passes into the renal tubule. The main function of the renal tubule is reabsorption. Reabsorption is the return of needed substances in the filtrate back to the bloodstream. It is necessary because some of the substances removed from the blood by filtration—including water, salts, glucose, and amino acids—are needed by the body. About 75 percent of these substances are reabsorbed in the renal tubule.
As shown in Figure 5, the renal tubule is divided into three parts: the proximal tubule, the Loop of Henle, and the distal tubule.
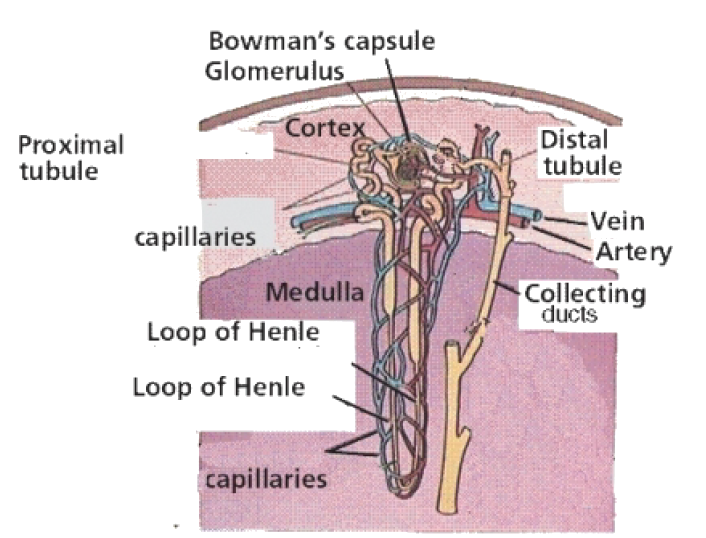
Figure 5: Parts of the renal tubule and other nephron structures.
• Filtrate first enters the proximal tubule. This is where that most reabsorption takes place. Tiny projections called microvilli line the proximal tubule and increase the surface area for reabsorption. From the proximal tubule, the filtrate passes through the loop of Henle.
• The loop of Henle carries the filtrate from the cortex down into the medulla and then back up to the cortex again. Its primary purpose is to reabsorb water and salt from the fluid. The remaining fluid enters the distal tubule.
• The distal tubule carries the fluid, now called tubular fluid, from the loop of Henle to a collecting duct. As it transports the fluid, the distal tubule also reabsorbs or secretes substances such as calcium and sodium. The process of secreting substances into the tubular fluid is called secretion.
Urine Formation
The collecting ducts are the site of urine formation. This process is crucial for water conservation in the body. The collecting ducts reabsorb water from tubular fluid and return it to the blood. The remaining fluid, called urine, has a smaller volume and a greater concentration than tubular fluid. From the collecting ducts, urine enters a ureter and is eventually excreted from the body.
The reabsorption of water by the collecting ducts is controlled by a negative feedback mechanism. The mechanism involves a hormone secreted by the pituitary gland, called antidiuretic hormone (ADH). ADH makes the collecting ducts more permeable to water, allowing more water to be reabsorbed from tubular fluid. When there is not enough water in the blood, more ADH is secreted, more water is reabsorbed from tubular fluid, and less water is excreted in urine. The opposite happens when there is too much water in the blood.
Kidneys and Homeostasis
The kidneys play many vital roles in homeostasis. As you have already read, the kidneys filter blood and excrete liquid waste. In fact, the kidneys filter all the blood in the body about 16 times a day, producing approximately 180 liters of filtrate and about 1.5 liters of urine. The kidneys also control the amount of water in the blood by excreting more or less water in urine.
Balancing the Blood
The kidneys are responsible for maintaining balance in the blood in other ways, as well. For example, they control the acid-base balance in the blood, mainly by secreting hydrogen ions into tubular fluid and reabsorbing bicarbonate ions from tubular fluid as needed. The kidneys also regulate blood concentrations of many other ions—including sodium, potassium, calcium, and magnesium—by the controlling the amounts that are excreted in urine.
Secreting Hormone
The kidneys also secrete various hormones to help maintain homeostasis. Hormones secreted by the kidneys include erythropoietin and rennin.
• Erythropoietin is secreted when the blood does not have enough red blood cells to carry adequate oxygen. The hormone stimulates the production of red blood cells by the bone marrow.
• Rennin is secreted when blood pressure falls. The hormone stimulates the secretion of aldosterone by the adrenal gland. Aldosterone, in turn, stimulates the kidneys to reabsorb more sodium ions and water. This increases the volume of the blood, which causes an increase in blood pressure.
Kidney Disease and Dialysis
A person can live a normal, healthy life with just one kidney. However, at least one kidney must function properly to maintain life. Diseases that threaten the health and functioning of the kidneys include kidney stones, infections, and diabetes.
Kidney Stones
Kidney stones are crystals of dissolved minerals that form in urine inside the kidneys. They may start out as small as a grain of salt and grow to be as large as a grapefruit. There may be one large stone or many small ones. Small kidney stones often pass undetected through the urinary tract and out of the body in urine. However, kidney stones may grow large enough before passing to block a ureter. This can cause a buildup of urine above the blockage and severe pain. Large kidney stones can sometimes be broken into smaller pieces that wash out of the urinary tract in urine. The stones are shattered by high-intensity sound waves focused on them from outside the body. Another alternative is to remove kidney stones surgically.
Infections
Bacterial infections of the urinary tract are very common. In fact, urinary tract infections (UTI) are the second most common type of bacterial infections seen by health care providers. Typical organisms that cause UTIs include Escherichia coli and Staphylococcus saprophyticus. The organisms may infect any part of the urinary tract.
The most common type of UTIs are bladder infections. They can be treated with antibiotics prescribed by a doctor. However, if a bladder infection is not treated, it may spread to the kidney and cause a kidney infection, or pyelonephritis. This is the most serious type of UTI. It can damage the kidney and interfere with normal kidney function. Kidney infections can also be treated with antibiotics but may require other treatments as well.
Diabetes
Two different types of diabetes can involve the kidneys: diabetes insipidus and diabetes mellitus. Diabetes insipidus is a disease characterized by the inability to concentrate urine. A person with this disease typically produces many liters of very dilute urine each day. Diabetes insipidus can be caused by a deficiency of ADH (antidiuretic hormone) or by the kidneys failing to respond to ADH. If the cause of diabetes insipidus can be treated, it may cure the disease.
In diabetes mellitus, the kidneys try to reduce the high glucose level in the blood by excreting more glucose in urine. This causes frequent urination and increased thirst. If blood glucose levels are not controlled by medication or diet, they may damage capillaries of the glomerulus and interfere with the kidney’s ability to filter blood. Eventually, high glucose levels may lead to kidney failure, in which kidney function is greatly reduced. Kidney failure leads to high levels of urea and other wastes in the blood and may require treatment with dialysis.
Dialysis and Transplantation
Dialysis is a medical procedure in which blood is filtered with the help of a machine. One type of dialysis treatment is shown in Figure 6. Blood from the patient’s vein enters the dialysis machine through a tube. Inside the machine, excess water, wastes, and other unneeded substances are filtered from the blood. The filtered blood is then returned to the patient’s vein through another tube. A dialysis treatment usually lasts three to four hours and must be repeated three times a week. Dialysis is generally performed on patients who have kidney failure. Dialysis helps them stay alive, but does not cure their failing kidneys.

Figure 6: Patient receiving dialysis treatment.
The only cure for most people with kidney failure is a kidney transplant. To be suitable for transplantation, the donated kidney must come from a donor who has the same blood and tissue types as the recipient. Even then, the recipient must take medication to suppress the immune system so it does not reject the new kidney.
Images courtesy of:
http://www.estrellamountain.edu/faculty/farabee/biobk/BioBookEXCRET.html. Public Domain.