The Endocrine System
Article objectives
The endocrine system is a system of organs that releases chemical message molecules, called hormones, into the blood. Unlike the nervous system whose action helps the body react immediately to change, such as quickly jumping out of the way of an oncoming cyclist, the endocrine system controls changes that happen to the body over a long period of time; from minutes, hours, to years of change. The two systems work closely together to help us respond to our environment, such as the rollercoaster ride shown in Figure 1. The endocrine system is important in controlling metabolism, growth and development, reproduction, and salt, water and nutrient balance of blood and other tissues (osmoregulation).
Function of the Endocrine System
The nervous system uses nerves to conduct electrical and chemical information around the body, while the endocrine system uses blood vessels to carry chemical information. You can think of the nervous system as being similar to the electrical system in a house. Flicking on a light switch is similar to initiating an action potential in a nerve, and it has an almost immediate result: the light bulb illuminates. The endocrine system on the other hand is more like starting up an oil or gas powered water-heating system. You flick on the switch to heat water up for a bath, but it takes a certain length of time for the result to occur: hot water.

Figure 1: What an adrenaline rush! The excitement that the people on this rollercoaster are feeling is a good example of how the nervous and endocrine systems work together. Nerve impulses from the sympathetic nervous system cause the adrenal medulla to release the hormone adrenaline into the bloodstream. Adrenaline causes the racing heart, sweaty palms, and feeling of alertness that together are called the ”fight or flight” response.
Organs of the Endocrine System
The endocrine system is made up of many glands that are located in different areas of the body. Hormones* are chemical messenger molecules that are made by cells in one part of the body and cause changes in cells in another part of the body. Hormones regulate the many and varied functions that keep you alive.
Hormones are made and secreted by cells in endocrine glands. Endocrine glands are ductless organs that secrete hormones directly into the blood or the fluid surrounding a cell rather than through a duct. The primary function of an endocrine gland is to make and secrete hormones. The endocrine glands collectively make up the endocrine system. The major glands of the endocrine system and their functions are shown in Figure 2. Many other organs, such as the stomach, heart, and kidneys secrete hormones and are considered to be part of the endocrine system.
Exocrine glands are organs that secrete their products into ducts (they are duct glands). They are similar to endocrine glands in that they secrete substances, but they do not secrete hormones. Instead they secrete products such as water, mucus, enzymes, and other proteins through ducts to specific locations inside and outside the body. For example, sweat glands secrete sweat onto the skin and salivary glands secrete saliva into the mouth. The reason we are discussing exocrine glands is because some endocrine glands, such as the pancreas, are also exocrine glands. Ducts in the pancreas secrete fatdigesting enzymes into the intestines. The secretion of the enzymes from the pancreas is controlled by hormones that are made by certain stomach cells.

Figure 2: The major organs of the endocrine system.
Hormones
The body produces many different hormones, but each hormone is very specific for its target cells. A target cell is the cell on which a hormone has an effect. Target cells are affected by hormones because they have receptor proteins that are specific to the hormone. Hormones will travel through the bloodstream until they find a target cell with the specific receptors to which they can bind. When a hormone binds to a receptor, it causes a change within the cell.
There are two main types of hormones, and a group of hormone-like substances:
• Amino Acid-Based Hormones
Amino acid-based hormones are made of amino acids. Some amino acid-based hormones are made of a few amino acids and are simple in structure while others are made of hundreds of amino acids and are very large. These hormones are not fat-soluble and therefore cannot diffuse through the plasma membrane of their target cell. They usually bind to receptors that are found on the cell membrane.
• Cholesterol-Based Hormones
Cholesterol-based hormones are made of lipids such as phospholipids and cholesterol. Hormones from this group are also called steroid hormones. Steroid hormones are fat soluble and are able to diffuse through the plasma membrane. Steroid hormone receptors are found within the cell cytosol and nucleus.
• Hormone-like Substances
The term hormone-like substances refers to a group of signaling molecules that are derived from certain types of fatty acids and proteins. Two examples of these substances are prostaglandins and neuropeptides. These substances do not travel around the body in blood as hormones do and tend to be broken down quickly. As a result, the effects of hormonelike substances are localized in the tissue in which it they are produced. For example, prostaglandins, which are made from essential fatty acids, are produced by most cells in the body. Prostaglandins have many different effects such as causing constriction or dilation of blood vessels but they are all are localized within the target cells and tissues. Neuropeptides are signaling peptides found in nervous tissue. Neuropeptides have many effects on nerve cells. For example, they can affect gene expression, local blood flow, and the shape of glial cells. Some neuropeptides such as endorphins and oxytocin have effects on non-nerve cells and are called hormones. Both signaling molecules have an effect on behavior. Among other things, endorphins are involved in pain perception and oxytocin is involved in social bonding and maternal behavior.
The cells that make hormones are usually specialized for the job, and are found within a particular endocrine gland, for example the thyroid gland, the ovaries, or the testes. Hormones may exit their cell of origin by exocytosis or another type of membrane transport. Typically cells that respond to a particular hormone may be one of several cell types that are found in different tissues throughout the body. Such is the case for insulin, which triggers a great number of physical effects. Different tissue types may also respond differently to the same hormonal signal. Because of this, hormonal signaling is a very complex process.
Hormone Receptors
Cells that respond to hormones have two properties in common: they have receptors that are very specific for certain hormones, and those receptors are joined with processes that control the metabolism of the target cells. There are two main ways that receptor-bound hormones activate processes within cells, depending on whether the hormone can pass across the membrane (steroid hormones are fat-soluble), or cannot pass through the membrane (most amino acid based hormones are water soluble).
• Second Messenger System
A water-soluble hormone molecule does not enter the cell, instead it binds to the membranebound receptor molecule, which triggers changes within the cell. These changes are activated by second messenger molecules.
• Direct Gene Activation
A fat-soluble hormone diffuses across the membrane and binds to the receptor within the cytosol or nucleus. The hormone-receptor complex then acts as a transcription factor that affects gene expression.
The two different ways that hormones can activate cells are discussed here, using the aminoacid based hormone glucagon and the steroid hormone cortisol as examples.
Action of Glucagon: A Second Messenger System
The majority of amino-acid based hormones, such as glucagon, bind to membrane-bound receptors. The binding of the hormone triggers a signal transduction pathway, a process of molecular changes that turns the hormone’s extracellular signal into an intracellular response. Activation of these receptors by hormones (the first messengers) leads to the intracellular production of second messengers as part of the signal transduction pathway. A second messenger is a small molecule that starts a change inside a cell in response to the binding of a specific signal to a receptor protein. Some second messenger molecules include small molecules such as cyclic AMP (cAMP), cyclic GMP (cGMP), and calcium ions (\(Ca^{2+}\)).
Glucagon is an important hormone involved in carbohydrate metabolism. It is released when the glucose level in the blood is low which causes the liver to change stored glycogen into glucose and release it into the bloodstream. Glucagon is released by the pancreas and circulates in the blood until it binds to a glucagon receptor, a G protein-linked receptor, found in the plasma membrane of liver cells. The binding of glucagon (first messenger) changes the shape of the receptor, which then activates a G protein. The G-protein is an enzyme that in turn activates the next enzyme in the cascade, the second messenger; adenylate cyclase. Adenylate cyclase produces cAMP which activates another enzyme, which in turn activates another enzyme, and so on. The end result is an enzyme that breaks apart the glycogen molecule in the liver cell to release glucose molecules into the blood. The signal transduction pathway, a type of enzyme “domino-effect” inside the cell, allows a small amount of hormone to have a large effect on the cell or tissue.
Action of Cortisol: A Direct Gene Activation
Steroid hormones diffuse through cell membrane and bind to receptors in the cytosol or the nucleus of the cell. The receptor-hormone complex acts as a transcription factor that affects gene expression.
Cortisol is a steroid hormone produced by the adrenal glands. It is often called the ”stress hormone” as it is involved in the body’s response to stress. It increases blood pressure, blood sugar levels and has an immunosuppressive action. Cortisol crosses the cell membrane and binds to a steroid receptor in the cytoplasm. The cortisol-receptor complex then enters the nucleus of the cell and binds to DNA, where it activates or deactivates gene transcription. The gene that is activated or deactivated depends on the cell type.
Effects of Hormones
The effects of hormones vary widely, and certain hormones, called tropic hormones (or tropins), regulate the production and release of other hormones. Many of the responses to hormones regulate the metabolic activity of an organ or tissue.
Other effects of hormones can include:
• Stimulation or inhibition of growth
• Induction or suppression of programmed cell death (apoptosis)
• Activation or inhibition of the immune system
• Regulation of metabolism
• Preparation for a new activity (e.g., fighting, fleeing, mating)
• Preparation for a new phase of life, for example puberty, caring for offspring, or menopause
• Control of the reproductive cycle
Hypothalamus and Pituitary Gland
The hypothalamus links the nervous system to the endocrine system by the pituitary gland. The hypothalamus is located below the thalamus, just above the brain stem. It is found in all mammalian brains, including humans. The human hypothalamus is about the size of an almond; its position in the brain is shown in Figure 40.

Figure 3: The hypothalamus is here. The red arrow shows the position of the hypothalamus in the brain.
The hypothalamus is a very complex area of the brain, and even small numbers of nerve cells within it are involved in many different functions. The hypothalamus coordinates many seasonal and circadian rhythms, complex homeostatic mechanisms, and the autonomic nervous system (ANS). A circadian rhythm is a roughly-24-hour cycle in the biological processes carried out within organisms, including plants, animals, fungi and certain bacteria. The ANS controls activities such as body temperature, hunger, and thirst. The hypothalamus must therefore respond to many different signals, some of which are from outside and some from inside the body. Thus, the hypothalamus is connected with many parts of the CNS, including the brainstem, the olfactory bulbs, and the cerebral cortex.
The hypothalamus produces hormones that are stored in the pituitary gland. For example, oxytocin and antidiuretic hormone (ADH) are made by nerve cells in the hypothalamus, and are stored in the pituitary prior to their release into the blood. In addition to influencing maternal behavior, oxytocin is involved in controlling circadian homeostasis, such as a person’s body temperature, activity level, and wakefulness at different times of the day. Antidiuretic hormone (ADH) is released when the body is low on water; it causes the kidneys to conserve water by concentrating the urine and reducing urine volume. It also raises blood pressure by causing blood vessels to constrict.
Pituitary Gland
The pituitary gland is about the size of a pea and is attached the hypothalamus by a thin stalk at the base of the brain, shown in Figure 4. The pituitary gland secretes hormones that regulate homeostasis. It also secretes hormones that stimulate other endocrine glands, called tropic hormones.

Figure 4: The position of the pituitary in the brain. A close-up of the anterior and posterior pituitary gland can be seen at right. The orange vessels are the capillary system that comes from the hypothalamus and carries hormones to the anterior pituitary (red) for storage. The blue vessels on the posterior pituitary come from the neurosecretory cells in the hypothalamus.
The anterior pituitary, or front lobe, makes many important hormones, which are listed in Table 1. The posterior pituitary, or rear lobe, releases two hormones, oxytocin and antidiuretic hormone (ADH) that are made by nerve cells in the hypothalamus. These hormones are transported down the nerve cell’s axons to the posterior pituitary where they are stored until needed.
Table 1: Pituitary Hormones
| Location | Hormone | Target | Function |
|---|---|---|---|
| Anterior Pituitary | Adrenocorticotropic hormone (ACTH) | Adrenal Gland | Stimulates adrenal cortex |
| Thyroid-stimulating hormone (TSH) | Thyroid Gland | Stimulates thyroid | |
| Growth hormone (GH) | Body cells | Growth hormone | |
| Follicle stimulating hormone (FSH) | Ovaries, Testes (Gonads) | Stimulates production of ovarian follicles in females, sperm production in males | |
| Leutinizing hormone (LH) | Ovaries, Testes | Causes ovulation in females | |
| Prolactin (PRL) | Ovaries, mammary glands | Causes milk secretion | |
| Posterior Pituitary | Anti diuretic hormone (vasopressin) | Kidneys or Arterioles uterus | Promotes water reabsorption in kidneys, raises blood pressure |
| Oxytocin | Mammary glands | Causes uterus to contract in childbirth, stimulates milk flow |
Most of these hormones are released from the anterior pituitary under the influence of hormones from the hypothalamus. The hypothalamus hormones travel to the anterior lobe down a special capillary system that surrounds the pituitary.
Oxytocin is the only pituitary hormone to create a positive feedback loop. For example, during the labor and delivery process, when the cervix dilates the uterus contracts. Uterine contractions stimulate the release of oxytocin from the posterior pituitary, which in turn increases uterine contractions. This positive feedback loop continues until the baby is born.
Other Endocrine Glands
Thyroid and Parathyroid Glands
The thyroid is one of the largest endocrine glands in the body. This butterfly-shaped gland is found in the neck, wrapped around the trachea, as shown in Figure 5. The hormones released by the thyroid control how quickly the body uses energy, makes proteins, and how sensitive the body should be to other hormones. The thyroid is controlled by the hypothalamus and pituitary. Thyroid hormone generally controls the pace of all of the processes in the body. This pace is related to your metabolism. If there is too much thyroid hormone, every function of the body tends to speed up. The thyroid gland regulates the body temperature by secreting two hormones that control how quickly the body burns calories. Hyperthyroidism (overactive thyroid) and hypothyroidism (under active thyroid) are the most common problems of the thyroid gland.

Figure 5: The position of the thyroid and parathyroid glands. A person can have more than four parathyroid glands.
The thyroid hormones thyroxine (T4) and triiodothyronine (T3) regulate the rate of metabolism and affect the growth and rate of function of many other systems in the body. As a result, problems with the under secretion or over secretion of thyroid hormones affect many body systems.
The element iodine is very important for making both T3 and T4. If a person’s diet does not have enough iodine, their thyroid cannot work properly and the person develops an iodine deficiency disease called goiter. Low amounts of T3 and T4 in the blood, due to lack of iodine to make them, causes the pituitary to secrete large amounts of thyroid stimulating hormone (TSH), which causes abnormal growth of the thyroid gland. The addition of small amounts of iodine to mass produced foods, such as table salt, has helped reduce the occurrence of iodine-deficiency in developed countries. The thyroid also produces the hormone calcitonin, which plays a role in calcium homeostasis. The hormones secreted by the thyroid are listed in Table 2.
Table 2: Hormones Secreted by the Thyroid and Parathyroid Glands
| Location | Hormone | Target | Function |
|---|---|---|---|
| Thyroid | Triiodothyroine (T3), Thyroxine (T4) | Body Cells | Increase metabolic rate, stimulates mental and physical growth |
| Calcitonin | Bone cells | Increases calcium absorption by bones, lowers blood calcium level | |
| Parathyroid | Parathyroid hormone (PTH) | Cells of the bone, kidney, and intestines | Regulates blood calcium levels |
Parathyroid Glands
The parathyroid glands are usually located behind the thyroid gland, but they are visible in Figure 5. Parathyroid hormone (PTH), maintains blood calcium levels within a narrow range, so that the nervous and muscular systems can work properly. When blood calcium levels drop below a certain point, calcium-sensing receptors in the parathyroid gland release the hormone parathyroid hormone (PTH) into the blood. PTH has effects that are opposite to the action of calcitonin. It increases blood calcium levels by stimulating certain bone cells to break down bone and release calcium. It also increases gastrointestinal calcium absorption by activating vitamin D, and promotes calcium uptake by the kidneys. The hormones secreted by the parathyroid glands are listed in Table 2.
Pineal Gland
The hormone melatonin is made in the pea-sized pineal gland, which is located at the base of the brain. Production of melatonin by the pineal gland is under the control of the hypothalamus which receives information from the retina about the daily pattern of light and darkness. Very little is currently known about the functions of melatonin, but scientists have found that it is involved in sleep cycles (circadian cycles), the onset of puberty, and immune function. Melatonin secretion also responds to seasonal changes in light, which could be a reason why getting out of bed on a dull, rainy morning can be so difficult, as the boy in Figure 6 probably knows.

Figure 6: Very little is currently known about the role of melatonin, but scientists do know that it is involved in sleep cycles. It is produced by the pineal gland, the retina and the intestines. Production of melatonin by the pineal gland is influenced of by the hypothalamus which receives information from the retina about the daily pattern of light and darkness.
Pancreas
The pancreas is both an exocrine gland as it secretes pancreatic juice containing digestive enzymes, and an endocrine gland as it produces several important hormones. It is located just below and behind the stomach, as shown in Figure 7. The endocrine cells of the pancreas are grouped together in areas called islets of Langerhans, shown in Figure 8. The islets produce the amino acid-based hormones insulin, glucagon, and somatostatin. Insulin and glucagon are both involved in controlling blood glucose levels. Insulin is produced by beta cells and causes excess blood glucose to be taken up by liver and muscle cells, where it is stored as glycogen, a polysaccharide. Glucagon is produced by alpha cells and stimulates liver cells to break down stores of glycogen into glucose which is then released into the blood. An alpha cell is another type of endocrine cell that is found within the islets of Langerhans. The hormones secreted by the pancreas are listed in Table 3.

Figure 7: The location of the pancreas in relation to the stomach and gall bladder. The hormone-producing Islet cells a found in groups throughout the pancreas.

Figure 8: Micrograph of an islet of Langerhans isolated from a rat pancreas. Each islet in a human pancreas contains approximately 1000 cells and is 50 to 500 micrometers in diameter. Cell nuclei are stained blue, insulin producing beta cells are green, and glucagonproducing alpha cells are red.
Table 3: Hormones Secreted by the Pancreas
| Hormone | Effects |
|---|---|
| Insulin | Reduces blood glucose concentration |
| Glucagon | Body Cells, Bone cells |
| Amylin | Body Cells, Bone cells |
| Somatostatin (inhibitory hormone) | Body Cells, Bone cells |
| Ghrelin | Body Cells, Bone cells |
Adrenal Glands
An adrenal gland is located above each of the kidneys, as shown in Figure 9. Each adrenal gland is separated into two structures, the adrenal medulla, which is the center of the gland, and the adrenal cortex, which is the outer layer. The medulla and the cortex work as two separate endocrine glands.

Figure 9: The location of the adrenal glands, above the kidneys.
The adrenal medulla is the core of the adrenal gland, and is surrounded by the adrenal cortex. Secretion of hormones from the medulla is controlled by the sympathetic nervous system. The cells of the medulla are the body’s main source of the hormones adrenaline (epinephrine) and noradrenaline (norepinephrine). These hormones are part of the fight-or-flight response initiated by the sympathetic nervous system. The hormone boosts the supply of oxygen and glucose to the brain and muscles, while suppressing other non-emergency bodily processes, such as digestion.
The adrenal cortex is the site of steroid hormone synthesis. Some cells make cortisol, while other cells make androgens such as testosterone. Other cells of the cortex regulate water and electrolyte concentrations by secreting aldosterone, which helps to regulate blood pressure. In contrast to the medulla that is controlled directly by the nervous system, the cortex is regulated by hormones secreted by the pituitary gland and hypothalamus.
Cortisol is an important steroid hormone that is often called the ”stress hormone” as it is involved in the response to stress, and is involved in restoring homeostasis after a stressful event, such as the (good) stress caused by running around a soccer field [football pitch (for non-American-English speakers)], shown in Figure 10. Cortisol increases blood pressure, blood sugar levels and has an immunosuppressive action. Long-term stress causes prolonged cortisol secretion, hyperglycemia, and weakening of the immune system. Excess levels of cortisol in the blood result in Cushing’s syndrome, symptoms of which include rapid weight gain, a round face, excess sweating, and thinning of the skin and mucous membranes.

Figure 10: Regular activity through sport is a good way of allowing your body to respond naturally to its stress hormones, which prepare the body for quick movements or prolonged activity.
Epinephrine, also called adrenaline, is a “fight or flight” hormone which is released from the adrenal medulla when stimulated by the sympathetic nervous system. Epinephrine plays a central role in the short-term stress reaction—the body’s response to threatening, exciting, or environmental stressors such as high noise levels or bright light. When secreted into the bloodstream, it binds to multiple receptors and has many effects throughout the body. Epinephrine increases heart rate, dilates the pupils, and constricts blood vessels in the skin and gut while dilating arterioles in leg muscles. It increases the blood sugar level, and at the same time begins the breakdown of lipids in fat cells. It also “turns down” non-emergency bodily processes such as digestion. Similar to other stress hormones, such as cortisol, epinephrine depresses the immune system.

Figure 11: Thinking about an upcoming exam can cause your adrenal glands to produce adrenaline (epinephrine). Your body’s stress response can cause you to feel “stressed out,” but can also motivate you to study.
Stress also releases norepinephrine in the brain. Norepinephrine has similar actions in the body as adrenaline, such as increasing blood pressure. Norepinephrine is also psychoactive because it affects alertness, which would be helpful for studying as shown in Figure 11. The hormones secreted by the adrenal cortex and medulla are listed in Table 3.
Table 4: Hormones of the Adrenal Glands
| Location | Hormone | Function |
|---|---|---|
| Adrenal Cortex | Mineralcorticoids (such as aldosterone) | Regulate sodium reabsorption and potassium elimination in the kidneys |
| Glucocortocoids (such as cortisol) | Depress immune response, provide stress resistance, helps in fat, protein and carbohydrate metabolism | |
| Gonadotropins | Stimulates releases of sex hormones that develop sexual characteristics of males and females | |
| Adrenal medulla | Epinephrine (adrenaline) | ”Fight or flight” hormone, plays central role in short-term response to stress, increases heart rate and supply of blood and oxygen to the brain |
| Norepinephrine (noradrenaline) | Increases alertness, physical effect similar to epinephrine |
Gonads
The ovaries of females and the testes of males are the gamete producing organs, or gonads. Ovaries in females are homologous to testes in males. In addition to producing gametes, an exocrine action, the gonads are endocrine glands that produce steroid sex hormones. Sex hormones are responsible for the secondary sex characteristics that develop at puberty. Puberty is the process of physical changes during which the sex organs mature and a person become capable of reproducing. During puberty, among other changes, males begin producing sperm and females begin menstrual cycles.
Luteinizing hormone (LH) and follicle stimulating hormone (FSH), which are both secreted by the pituitary gland, are called gonadotropes because they are tropic hormones of the gonads. Recall that tropic hormones trigger the production of hormones in other endocrine glands. The secretion of LH and FSH are, in turn, controlled by gonadotropin-releasing hormone for the hypothalamus. Those pulses, in turn, are subject to the estrogen feedback from the gonads.
In males LH triggers the production of sex hormones called androgens in the testes. The main androgen produced by the testes is testosterone. Testosterone causes an increase in skeletal muscle mass and bone density and is also responsible for the secondary sex characteristics of males such as facial hair, shown in Figure 12. The testes also produce small amounts of estrogen in the form of estradiol, which is believed to be important for sperm formation. On average, the human adult male body produces about eight to ten times more testosterone than an adult female body.

Figure 12: The male hormone testosterone stimulates the growth of facial hair. Many men develop facial hair in the later years of puberty, usually between the ages of 15 to 18 years. The amount of facial hair on a man’s face varies between individuals, and also between ethnic groups. For example, men from many East Asian or West African backgrounds typically have much less facial hair than those of Western European, Middle Eastern, or South Asian descent.

Figure 13: Maintaining correct hormone levels (especially progesterone), throughout pregnancy is important for carrying a pregnancy to full term.
In females a rise in LH concentration triggers the production of estrogen and progesterone by the ovaries. Estrogen causes the release of an egg from the ovaries and progesterone prepares the uterus for a possible implantation by a fertilized egg. The placenta is an endocrine gland of pregnancy because it secretes the hormones estrogen, human chorionic gonadatropin, and progesterone which are important for maintaining a pregnancy, shown in Figure 13. The hormones secreted by the male and female gonads are listed in Table 5.
Table 5: Hormones Secreted by Gonads
| Organ | Hormone | Target | Function |
|---|---|---|---|
| Ovaries | Estrogen | Bone cells, cells of sex organs | Promotes growth and development of female sex organs; Maintains uterine lining |
| Testes | Progesterone, Testosterone | Bone cells, muscle cells, cells of sex organs | Stimulates growth and development of male sex organs and sex drive |
Other Hormone-Producing Tissues and Organs
Several organs that are generally nonendocrine in function, such as the stomach, the small intestine, the kidneys, and the heart have cells that secrete hormones. For example, the kidneys secrete erythropoietin (EPO), a hormone that regulates red blood cell production, and the heart secretes atriopeptin, a hormone that reduces water and sodium levels in the blood, which decreases blood pressure. Ghrelin is a hormone that stimulates appetite and is produced by certain cells that line the stomach. Certain cancer cells secrete hormones that can interfere with homeostasis.
Regulation: Feedback Mechanisms
Hormones regulate many cell activities and so are important to homeostatic regulation. The rate of hormone production and secretion is often controlled by homeostatic feedback control mechanisms, and the effect of hormones is also controlled by hormone antagonists. In these ways, the concentration of hormones and their products is kept within a narrow range so as to maintain homeostasis.
A feedback control mechanism, or a feedback loop, is a signaling system in which a product or effect of the system controls an earlier part of the system, either by shutting the process down or speeding it up. Most feedback mechanisms of the body are negative, only a few are positive. Hormone antagonists and hormone receptor antagonists are hormones or other molecules that block the action of hormones, and are also used by the body to control the action of hormones.
Negative Feedback
Negative feedback is a reaction in which the system responds in such a way as to reverse the direction of change. Since this tends to keep things constant, it allows for a process to return from a state of imbalance back to a homeostatic equilibrium.
A common, non-biological example of negative feedback happens in a home heating system. When you are home, you set your thermostat to 21˚C (about 70˚F), which is the set point. The thermometer in the thermostat monitors the room temperature and will sense when the temperature drops below the 21˚C set point (the stimulus). The thermometer will then send a message to the thermostat (control center), which in turn sends a message to the furnace to switch on and heat up the room. When the room temperature returns to the set temperature, the thermostat shuts the furnace off. In this home-heating example, the increase in air temperature is the negative feedback that results in the furnace being shut off. In this way a set room temperature of 21˚C (within a degree or two) is maintained.
An example of negative feedback in the body is the control of blood-glucose concentrations by insulin. A higher amount of glucose in the blood (the stimulus), signals the beta cells of the pancreas to release insulin into the blood. Hormone concentration alone cannot trigger a negative feedback mechanism, negative feedback is instead triggered by an overproduction of the effect of the hormone, such as the lowering of blood glucose concentration (the effect), which causes a decrease in the secretion of insulin by the pancreas.
Negative Feedback: Regulation of Thyroid Hormone
The thyroid hormones thyroxine (T4) and triiodothyronine (T3) regulate the rate of metabolism. The production of T4 and T3 is regulated by a thyroid-stimulating hormone (TSH), which is released by the anterior pituitary. The thyroid and the TSH-producing cells of the anterior pituitary form a negative feedback loop, as shown in Figure 14.
Thyroid-stimulating hormone production is decreased when the T4 levels are high, and when TSH levels are high, T4 production is decreased. The production and secretion of TSH is in turn controlled by thyrotropin-releasing hormone (TRH), which is produced by the hypothalamus. The rate of TRH secretion is increased in situations such as cold temperature because increasing the metabolic rate would generate more heat. Increased levels of T4 and T3 in the blood cause a reduction in TRH secretion. Among other things, TSH secretion is reduced by high levels of thyroid hormones, as well as the antagonistic hormone somatostatin. These feedback loops keep the concentration of thyroid hormones within a narrow range of concentrations.
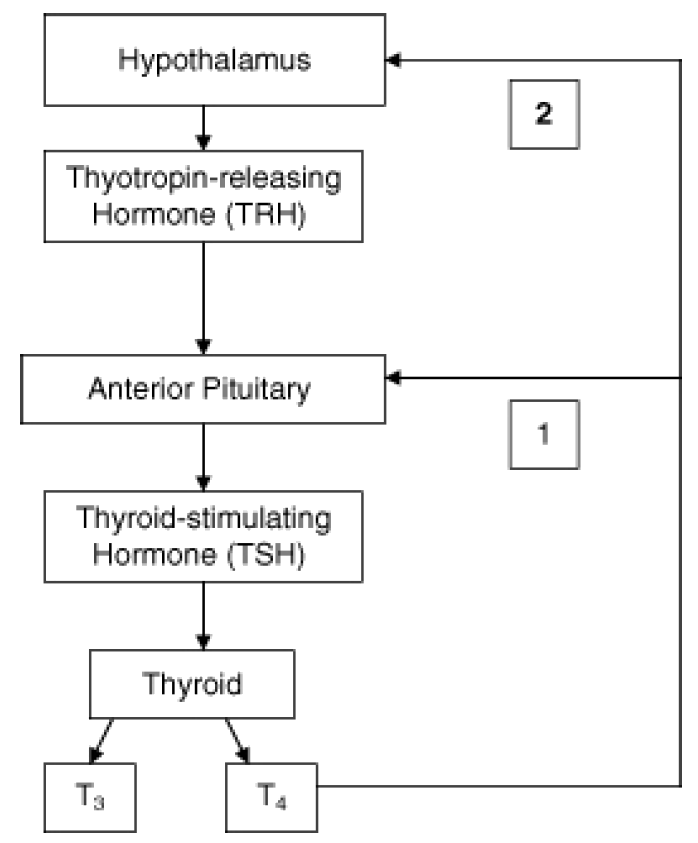
Figure 14: Two negative feedback loops exist in the control of thyroid hormone (1) shows the loop between the TSH-producing cells of the anterior pituitary and the thyroid. Increased levels of T4 and T3 in the blood cause a reduction in TSH secretion. (2) shows that increased levels of T4 and T3 in the blood cause a reduction in TRH secretion.
Positive Feedback
Positive feedback is a reaction in which the system responds in such a way as to speed up the direction of change. Positive feedback mechanisms are not as common as negative feedback mechanisms because they cause an increase in the initial signal, which would tend to knock many systems out of balance. Take for example, the analogy of the home heating system. If this system were to work on a positive feedback loop, the furnace would not switch off when the temperature reached the set point of 21˚C. Instead, it would keep going and heat the room indefinitely.
An example of a positive feedback mechanism is milk production by a mother for her baby, as shown in Figure 15. As the baby suckles, nerve messages from the mammary glands cause the hormone prolactin, to be secreted by the mother’s pituitary gland. The more the baby suckles, the more prolactin is released, which stimulates further milk production by the mother’s mammary glands. In this case, a negative feedback loop would be unhelpful because the more the baby nursed, the less milk would be produced. Another example of a positive feedback loop is the blood-clotting cascade that happens after a blood vessel is cut.

Figure 15: Production of breast milk is controlled by a positive feedback mechanism.
Hormone Antagonists
Many hormones work with hormone antagonists to control the concentrations of substances in the body. The hormones have opposite actions on the body and so are called antagonistic.
Insulin and glucagon make up an antagonistic hormone pair. The action of insulin is opposite that of glucagon. For example, your blood glucose concentration rises sharply after you eat food that contains simple carbohydrates, such as the blueberry muffins shown in Figure 16. The increase in blood glucose level stimulates beta cells in the pancreas to release insulin into blood. In response to signals by insulin most body cells take up glucose, which removes it from the blood, and the blood glucose concentration returns to the set point. Later, you have missed eating lunch, you are hungry and feel a little light headed. Your blood glucose concentration has dropped below the set point, which causes the release of glucagon from the pancreas. Glucagon causes the release of glucose from liver cells, which increases your blood-glucose concentration. If glucagon did not do its job correctly, your blood glucose concentration would continue to drop, and you would develop hypoglycemia (low blood sugar). This antagonistic relationship between the two hormones helps to maintain the narrow range of blood glucose concentration.

Figure 16: Insulin and glucagon work as an antagonistic pair to keep your blood glucose concentration within a narrow range even after you eat food containing carbohydrates, such as a muffin.
The actions of growth hormone releasing hormone (GHRH) are opposed by another hypothalamic hormone, somatostatin, also known as ”growth-hormone-inhibiting hormone” (GHIH). Somatostatin and GHRH are secreted alternatively by the hypothalamus, which causes an increase and decrease in the secretion of growth hormone (GH) by the pituitary.
Many endocrine glands also work together as a group to control body processes. The major endocrine glands coordinate the control of various regulatory systems, such as metabolism, osmoregulation, and reproduction. Many individual glands are directly controlled by the nervous system, and all are in some way controlled by the pituitary and hypothalamus. Some of these glands and their hormone products are listed in Table 6.
Table 6: Coordination of the Endocrine Glands in the Control of Body Systems
| Function | Organ or Glands | Hormones | Nervous System Control |
|---|---|---|---|
| Control of the Endocrine System | Hypothalamus Pituitary Gland | TSH, FSH, LH, GH, prolactin (PRL); Adrenocorticotropic hormone (ACTH) | ANS (sympathetic and parasympathetic nervous system) |
| Regulation of Metabolism | Thyroid Gland, Parathyroid Glands, Pancreas, Pineal Gland, Liver | \(T_3\) and \(T_4\) Parathyroid hormone, Insulin, Glucagon, Melatonin | ANS (sympathetic and parasympathetic nervous system) |
| Response to Stress | Adrenal Glands | Epinepherine, norepinepherine, cortisol | ANS (sympathetic nervous system) |
| Reproduction | Gonads (ovaries, testes) | Androgens (testosterone), estrogens, progestins (progesterone) | ANS (parasympathetic nervous system) |
| Osmoregulation | Adrenal Glands, Kidneys, Liver | Aldosterone, ADH, Angiotensin | ANS (sympathetic and parasympathetic nervous system) |
Homeostatic Imbalance: Endocrine System Disorders
Diseases of the endocrine system are common, and include diseases such as diabetes, thyroid disease, and obesity. An endocrine disease is usually characterized by hyposecretion or hypersecretion of hormones and an inappropriate response to hormone signaling by cells.
Cancer can occur in endocrine glands, such as the thyroid, and some hormones are involved in signaling distant cancer cells to multiply. For example, the estrogen receptor has been shown to be involved in certain types of breast cancers.
Hyposecretion
Hyposecretion is the production no hormone or too little of a hormone. It can be caused by the destruction of hormone-secreting cells, such as in Type 1 diabetes, or by a deficiency in a nutrient that is important for hormone synthesis. Hyposecretion can be treated with hormone-replacement therapies. Type 1 diabetes is an autoimmune disease that results in the destruction of the insulin-producing beta cells of the pancreas. A person with Type 1 diabetes needs insulin replacement therapy, usually by injection or insulin pump, in order to stay alive. An insulin pump is shown in Figure 17.

Figure 17: In the treatment of Type 1 diabetes, an insulin pump is an alternative to multiple daily injections of insulin. The pump is usually used along with the monitoring of blood glucose concentration and carbohydrate intake.
Diabetes insipidus is characterized by excretion of large amounts of very dilute urine, even if liquid intake is reduced. It is caused by an inability of the kidney to concentrate urine due to a lack of antidiuretic hormone (ADH) also called vasopressin, or by an insensitivity of the kidneys to that hormone. Blood glucose levels are not affected in diabetes insipidus.
Growth hormone deficiency is caused by a lack of GH production by the pituitary. GH deficiency affects bone growth development, and people with growth hormone deficiency tend to have, among other things, low bone density and small stature, a condition called pituitary dwarfism. GH deficiency is treated by growth hormone replacement.
Hypothyroidism is the state in which not enough thyroid hormones are made. Thyroiditis is an autoimmune disease where the body’s own antibodies attack the cells of the thyroid and destroy it. Thyroid hormones play an important role in brain development during fetal growth. Cells of the brain are a major target for the T3 and T4 hormones. As a result, hypothyroidism in children, either due to a thyroid problem from birth or a lack of iodine in the diet, is a major cause of physical and mental growth impairment in developing countries. In fact, iodine deficiency disorders are the single most common cause of preventable mental retardation and brain damage in the world.
Hypersecretion
Hypersecretion of a hormone happens when the body produces too much of a hormone. A hormone can be hypersecreted if the gland develops a tumor and grows out of control, or if the gland is signaled to produce too much of a hormone.
Hyperthyroidism is the result of excess thyroid hormone production, which causes an overactive metabolism and increased speed of all the body’s processes. Hyperthyroidism is the most common cause of goiter in the developed world, shown in Figure 18.

Figure 18: There are many causes of goiter, but the most common is the world is iodine deficiency. Today, iodine deficiency remains mostly a problem in poorer countries which lack the means to add iodine to foods. Iodized salt has helped reduce the amount of iodine deficiency in the developed world. Governments of some countries add iodine to cattle feed to ensure that dairy foods will contain iodine.
Hypersecretion of growth hormone causes acromegaly. A common cause of acromegaly is a benign tumor of the pituitary glands that releases too much GH. In some cases, acromegaly is also caused by overproduction of the hypothalamus hormone growth hormone release hormone (GHRH). Acromegaly most commonly affects middle-aged adults and can result in serious illness and premature death. Symptoms include enlarged hands and feet, protruding brow and chin, and enlarged internal organs. However, the disease is hard to diagnose in the early stages and is frequently missed for many years due to its slow progression. If the pituitary produced too much GH during childhood, the person will be taller than normal, a condition called pituitary gigantism. Pituitary gigantism is very rare, and some of the tallest people on record had this condition.
Hormone Insensitivity: Type 2 Diabetes
In some cases, the body makes enough hormones, but body cells do not respond. This can be due to missing or defective hormone receptors, or the body cells become resistant to normal concentration of the hormone, and do not respond to it.
Type 2 diabetes is characterized by hyperglycemia (high blood glucose concentrations), body cells that do not respond to normal amounts of insulin (insulin resistance), and the resulting inability of the pancreas to produce enough insulin. Insulin resistance in cells results in high amounts of free fatty acids and glucose in the blood. High plasma levels of insulin and glucose due to insulin resistance often lead to metabolic syndrome and Type 2 diabetes. Type 2 diabetes can be controlled by improving the diet, increasing levels o activity, and sometimes medication.
Gestational diabetes is a form of diabetes that affects pregnant women. There is no known single cause, but it’s believed that the hormones produced during pregnancy reduce the ability of the cells in the pregnant woman’s body to respond to insulin, which results in high blood glucose concentrations.
Hormones as Medicines
Many hormones and molecules like them are used as medicines. The most common type of therapy is called hormone-replacement therapy. The most commonly-prescribed hormones are estrogens and synthetic progesterone (as methods of hormonal contraception and as HRT therapy for post-menopausal women), thyroxine (as levothyroxine, for hypothyroidism) and corticosteroids (for autoimmune diseases and several respiratory disorders). Progestin, a synthetic progesterone, is also used to prolong pregnancy in women who have experienced a miscarriage due to a premature drop in progesterone levels. Hydrocortisone is a synthetic form of cortisol that is used to treat allergies and inflammation as well as cortisol production deficiencies. Hydrocortisone cream is a common over-the-counter medication for the topical treatment of rash. Insulin is used by many people with diabetes.
Epinephrine
Because of its anti inflammatory effect on the immune system, epinephrine is used to treat anaphylaxis. Anaphylaxis is a sudden and severe allergic reaction that involves the entire body. After an initial exposure to a substance like a certain food (such as peanuts), or bee sting, a person’s immune system can becomes sensitized to that substance, which is called an allergen. Upon second exposure, an allergic reaction occurs.

Figure 19: An EpiPen® epinephrine autoinjector. Auto injectors like this one can help save a person’s life during an anaphylactic reaction.
Histamine and other substances that are released by body cells cause the blood vessels to dilate, which lowers blood pressure, and fluid to leak from the bloodstream into the tissues, which lowers the blood volume. The release of histamine causes the face and tongue to swell. Swelling of the lining of the throat can lead to breathing difficulties. The hormone epinephrine causes blood vessels to constrict which reduces swelling and causes blood pressure to increase. Epinephrine is used as a medicine in auto injectors, shown in Figure 19, which a person can use themselves should they have an anaphylactic reaction.
Anabolic Androgenic Steroids
Synthetic androgens, in the form of anabolic androgenic steroids (anabolic steroids), have many medical uses. It is used to stimulate bone growth and appetite, induce puberty in boys, and treat muscle-wasting conditions in patients that have diseases such as cancer and AIDS. In general, androgens, including testosterone, promote protein synthesis and the growth of muscle tissue and other tissues that have androgen receptors. Androgens also block the effects of the stress hormone cortisol on muscle tissue, so the breakdown of muscle is greatly reduced.

Figure 20: Athletes involved in sports that emphasize strength, weight, and shape may feel pressure to take anabolic steroids, however, the majority of school athletes do not take them.
Anabolic Steroid Abuse
As a result of their muscle-building action, anabolic steroids are used in sport and bodybuilding to increase muscle size and strength, to gain a competitive edge or to assist in recovery from injury. Steroids used to gain competitive advantage are forbidden by the rules of the governing bodies of many sports. Serious health risks can be produced by long-term use or excessive doses of anabolic steroids. Most of these side effects are dose dependent, the most common being an increase in low density lipoprotein (bad cholesterol), and a decrease in good high density lipoprotein (good cholesterol). Anabolic steroids also increase the risk of cardiovascular disease in men with high risk of bad cholesterol. Acne is fairly common among anabolic steroid users, mostly due to increases in testosterone which stimulates the sebaceous glands to produce more oil. High doses of anabolic steroids have been linked to liver damage.
Teenagers, particularly boys, who take anabolic steroids, are more likely to be involved in sports that emphasize weight and shape, (such as football or wrestling, which is shown in Figure 20). Such teens also have higher rates of disordered eating, drug abuse, and generally have poorer attitudes towards health. Severe side effects can occur if a teenager uses anabolic steroids. For example, the steroids may prematurely stop the lengthening of bones, resulting in stunted growth. Other effects include, but are not limited to, accelerated bone maturation, increased acne outbreaks, and premature sexual development.
In addition to dangerous side effects of the steroids themselves, dangerous drug-taking habits that have been reported by abusers include: unsafe injection practices such as reusing needles, sharing needles, and sharing multidose vials. A common practice among anabolic steroid abusers is self–medicating with other hormones such as growth hormone and insulin, which in itself can lead to serious health consequences. Testosterone and other anabolic steroids are classified as a controlled substance in the United States (US), Canada, the United Kingdom (UK), Australia, Argentina, and Brazil.
Images courtesy of:
http://www.flickr.com/photos/sfllaw/509150616/. CC-BY-SA 2.0.
http://commons.wikimedia.org/wiki/Image:Hypothalamus.jpg. Public Domain.
Pituitary gland: http: //training.seer.cancer.gov/module_anatomy/unit6_1_endo_intro.html. Public Domain.
USFG. http://en.wikipedia.org/wiki/Image:Illu_thyroid_parathyroid.jpg. Public Domain.
http://www.flickr.com/photos/cliche/120050450/. CC-BY-SA-2.0.
http://training.seer.cancer.gov/anatomy/endocrine/glands/pancreas.html. Public Domain.
http://commons.wikimedia.org/wiki/Image:Pancreaticislet.jpg. CC-BY-SA.
http://training.seer.cancer.gov/anatomy/endocrine/glands/adrenal.html. Public Domain.
adobemac. http://www.flickr.com/photos/adobemac/257761265/in/photostream/. CC-BY-SA 2.0.
Aaron Jacobs. http://www.flickr.com/photos/aaronjacobs/64657662/. CCBy- SA 2.0.
http://www.flickr.com/photos/marklarson/418292246/. CC-BY-SA 2.0.
http://www.flickr.com/photos/mahalie/144905384/. CC-BY-SA-2.0.
Nabeel H. http://www.flickr.com/photos/nabeel/16876576/. CC-BY-SA 2.0.
Pansonaut. http://www.flickr.com/photos/pansonaut/208125336/. CC-BYSA- 2.0.
M. Bradford. http://en.wikipedia.org/wiki/Image:Insulin_pump_with_infusion_set.jpg. Public Domain.
Martin Finborud. http://en.wikipedia.org/wiki/Image:Kone_med_stor_struma.jpg. Public Domain.
Sean William. http://commons.wikimedia.org/wiki/Image:Epipen.jpg. GNU-FDL.
washer_dreier. http://www.flickr.com/photos/washer/314535942/. CC-BY-SA-2.0.