Circulatory System
Article objectives
The cardiovascular system shown in Figure 1 is an organ system that moves nutrients, hormones, gases and wastes to and from body cells, and distributes heat to maintain homeostasis. The main components of the cardiovascular system are the heart, the blood vessels, and the blood.
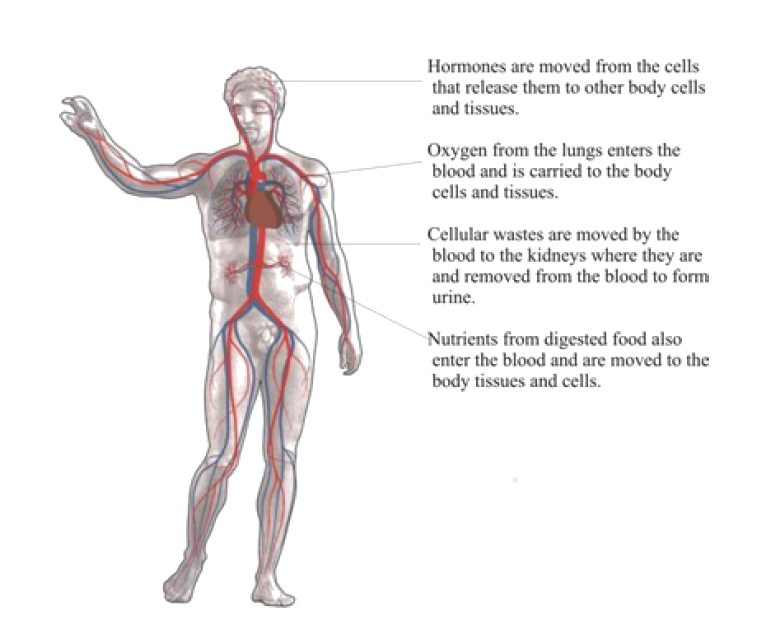
Figure 1: The main organs of the circulatory system. Blood acts as the transporter in the body, while blood vessels act like little (one way) roads. The figure is Michelangelo’s marble sculpture David, which does not actually have a circulatory system.
The Heart
The heart is the muscular organ that pumps blood through the blood vessels by repeated, rhythmic contractions. The term cardiac means ”related to the heart” and comes from the Greek word kardia, for ”heart.” The heart is made up mostly of cardiac muscle tissue, (shown in Figure 2) which contracts to pump blood around the body. In adults, the normal mass of the heart is 250-350 grams (9-12 oz), or about three quarters the size of a clenched fist, but badly diseased hearts can be up to 1000 g (2 lb) in mass due to enlargement of the cardiac muscle.
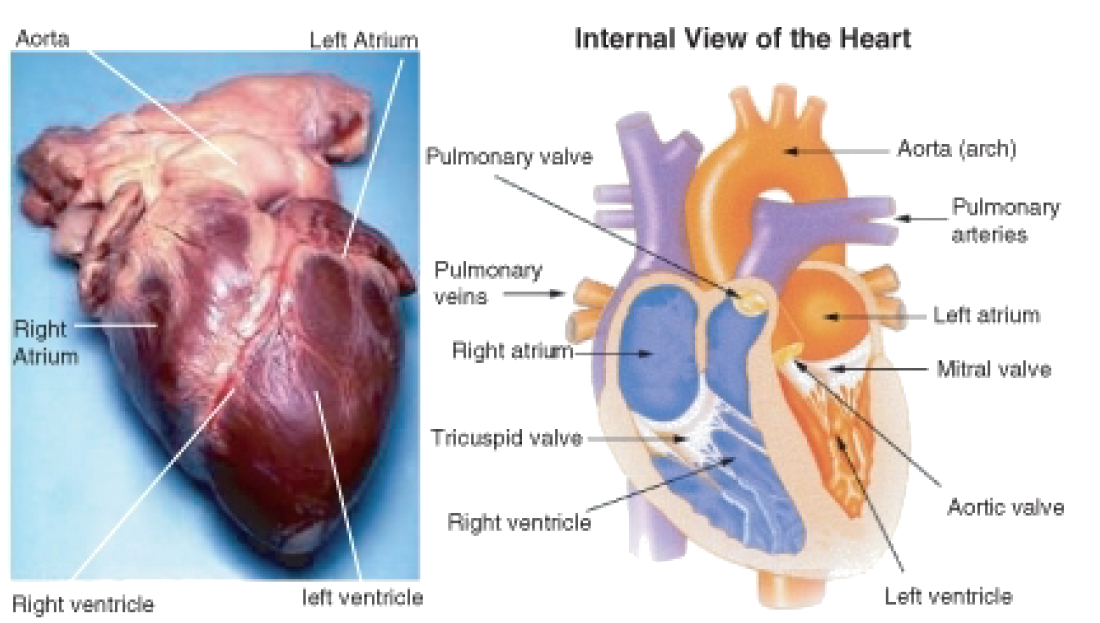
Figure 2: External and internal views of the human heart. The aorta in the photo cannot be seen clearly because it is covered by a layer of adipose tissue (fat).
The heart is usually found in the left to middle of the chest with the largest part of the heart slightly to the left. The heart is usually felt to be on the left side because the left ventricle is stronger (it pumps to all the body parts). The heart is surrounded by the lungs. The left lung is smaller than the right lung because the heart takes up more room in the left side of the chest. The position of the heart within the chest is shown in Figure 3.

Figure 3: Position of the heart in relation to the lungs. The heart can be seen in the lower middle area of the figure, behind the lungs.
Blood Flow Through the Heart
Blood flows through the heart in two separate loops; you could think of them as a “left side loop” and a “right side loop.” The right side and left side of the heart refer to your heart as it sits within your chest. Its left side is your left side and, its right side is your right side.
The right side of the heart collects deoxygenated blood from the body and pumps it into the lungs where it releases carbon dioxide and picks up oxygen. The left-side carries the oxygenated blood back from the lungs, into the left side of the heart which then pumps the oxygenated blood throughout the rest of the body.
The heart has four chambers, the two upper atria and the two lower ventricles. Atria (singular, atrium) are the thin-walled blood collection chambers of the heart. Atria pump the blood into the ventricles. Ventricles are the heart chambers which collect blood from the atria and pump it out of the heart. On the right side of the heart, deoxygenated blood from the body enters the right atrium from the superior vena cava and the inferior vena cava, shown in Figure 4. Blood enters the right ventricle which then pumps the blood through the pulmonary arteries and into the lungs. In the lungs, carbon dioxide is released from the blood and oxygen is picked up.
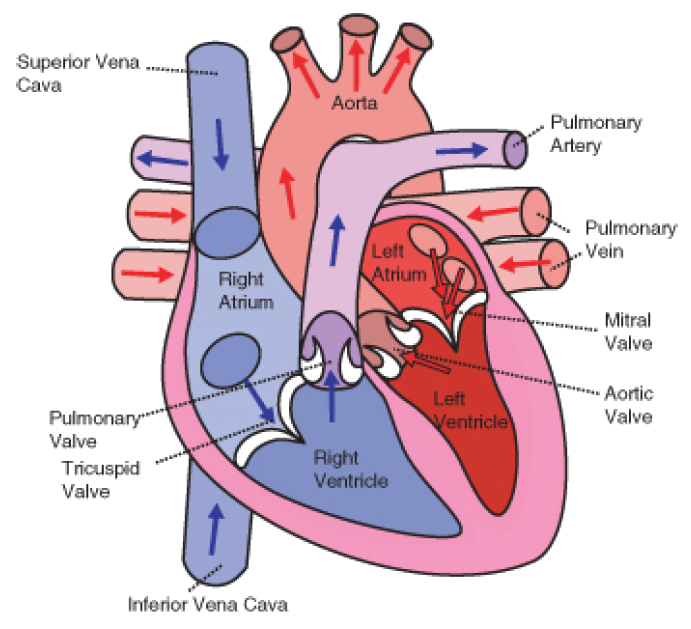
Figure 4: The direction of blood flow through the heart.
Pulmonary veins bring the oxygenated blood back to the heart and into the left atrium. From the left atrium the blood moves to the left ventricle which pumps it out to the body through the aorta. On both sides, the lower ventricles are thicker and stronger than the upper atria. The muscle wall surrounding the left ventricle is thicker and stronger than the wall surrounding the right ventricle because the left ventricle needs to exert enough force to pump the blood through the body. The right ventricle only needs to pump the blood as far as the lungs, which does not require as much contractile force.
Valves in the heart maintain the flow of blood by opening and closing in one direction only. Blood can move only forward through the heart, and is prevented from flowing backward by the valves. Such movement of the blood is called unidirectional flow. There are four valves of the heart:
• The two atrioventricular (AV) valves ensure blood flows from the atria to the ventricles, and not the other way. The AV valve on the right side of the heart is called the tricuspid valve, and the one on the left of the heart is called the mitral, or bicuspid valve.
• The two semilunar (SL) valves are present in the arteries leaving the heart, and they prevent blood flowing back from the arteries into the ventricles. The SL valve on the right side of the heart is called the pulmonary valve, because it is leads to the pulmonary arteries, and the SL valve on the left is called aortic valve because it leads to the aorta. The valves of the heart are shown in Figure 4.
The Heartbeat
The heart is a meshwork of cardiac muscle cells that are interconnected by little channels called gap junctions. This interconnection allows the electrical stimulation of one cell to spread quickly to its neighboring cells. Cardiac muscle is self-exciting. This is in contrast to skeletal muscle, which needs nervous stimulation to contract. The heart’s rhythmic contractions occur spontaneously, although the frequency of the contractions, called the heart rate, can be changed by nervous or hormonal signals such as exercise or the perception of danger.
Control of the Heartbeat
The rhythmic sequence of contractions of the heart is coordinated by two small groups of cardiac muscle cells called the sinoatrial (SA) and atrioventricular (AV) nodes. The sinoatrial node (SA node), often known as the ”cardiac pacemaker”, is found in the upper wall of the right atrium and is responsible for the wave of electrical stimulation that starts atrial contraction by creating an action potential. The action potential causes the cardiac cells to contract. This wave of contraction then spreads across the cells of the atrium, reaching the atrioventricular node (AV node) which is found in the lower right atrium, shown in Figure 5. The AV node conducts the electrical impulses that come from the SA node through the atria to the ventricles. The impulse is delayed there before being conducted through special bundles of heart muscle cells called the bundle of His and the Purkinje fibers, which leads to a contraction of the ventricles. This delay allows for the ventricles to fill with blood before the ventricles contract. Heartbeat is also controlled by nerve messages originating from the autonomic nervous system.

Figure 5: Schematic representation of the atrioventricular Bundle of His. The SA node is blue, and the AV node is red and visible in the right atrium. The AV node forms the Bundle of His. Sometimes the left and right Bundles of His are called Purkinje fibers.
There are important physiological differences between cardiac cells found in the nodes and cardiac cells found in the ventricles. Differences in ion channels and mechanisms of polarization give rise to unique properties of SA node cells, most importantly the spontaneous depolarizations necessary for the SA node’s pacemaker activity.
The Bundle of His is a collection of heart muscle cells (fibers) specialized for electrical conduction that transmits the electrical impulses from the AV node. The bundle of His branches into Purkinje fibers. Purkinje fibers, shown in Figure 6, are specialized cardiac muscle cells that conduct action potentials into the ventricles, causing the cardiac muscle of the ventricles to contract in a controlled way.

Figure 6: The larger round cells on the right are Purkinje fibers. Because of their specializations to rapidly conduct impulses (numerous sodium ion channels and mitochondria, fewer myofibrils than the surrounding muscle tissue), Purkinje fibers take up stain differently than the surrounding muscles cells, and on a slide, they often appear lighter and larger than their neighbors.
The heartbeat is made up of two parts; muscle contraction and relaxation. Systole is the contraction of the heart chambers, which drives blood out of the chambers. Diastole is the period of time when the heart relaxes after contraction. All four chambers of the heart undergo systole and diastole in a timed fashion so that blood is moved forward through the cardiovascular system. For example, ventricular systole is the point at which the ventricles are contracting, and atrial systole is the point at which the atria are contracting. Likewise, ventricular diastole is the period during which the ventricles are relaxing, while atrial diastole is the period during which the atria are relaxing. In general, when referring to systole and diastole, the chambers being referred to are the ventricles, which is shown in Figure 7.

Figure 7: When the atria contract, the blood gets pushed into the ventricles which are in diastole. When the ventricles contract (ventricular systole), the blood gets pushed out of the heart.
Heart Sounds
In healthy adults, there are two normal heart sounds often described as a ”lub” and a ”dub” that occur with each heart beat (lub-dub, lub-dub). In addition to these normal sounds, a variety of other sounds may be heard including heart murmurs or clicks. A medical practitioner uses a stethoscope to listen for these sounds, which gives him or her important information about the condition of the heart.
The sound of the heart valves shutting causes the heart sounds, or a heartbeat. The closing of the mitral and tricuspid valves (known together as the atrioventricular valves) at the beginning of ventricular systole cause the first part of the ”lub-dub” sound made by the heart as it beats. The second part of the ”lub-dub” is caused by the closure of the aortic and pulmonic valves at the end of ventricular systole. As the left ventricle empties, its pressure falls below the pressure in the aorta, and the aortic valve closes. Similarly, as the pressure in the right ventricle falls below the pressure in the pulmonary artery, the pulmonic valve closes.
Blood Vessels
The blood vessels are part of the cardiovascular system and function to transport blood throughout the body. The two most important types are arteries and veins. Arteries carry blood away from the heart, while veins return blood to the heart.
There are various kinds of blood vessels, the main types are:
• Arteries are the large, muscular vessels that carry blood away from the heart.
• An arteriole is a small diameter blood vessel that extends and branches out from an artery and leads to capillaries.
• Veins are vessels that carry blood toward the heart. The majority of veins in the body carry low-oxygen blood from the tissues back to the heart.
• A venule is a small vessel that allows deoxygenated blood to return from the capillaries to veins.
• Capillaries are the smallest of the body’s blood vessels, that connect arterioles and venules, and are important for the interchange of gases and other substances between blood and body cells.
The blood vessels have a similar basic structure. The endothelium is a thin layer of cells that creates a smooth lining on the inside surface of blood vessels. Endothelial tissue is a specialized type of epithelium, one of the four types of tissue found in the body. Endothelial cells have an important structural role in blood vessels; they line the entire circulatory system, from the heart to the smallest capillary. Around the endothelium there is a layer of smooth muscle, which is well developed in arteries. Finally, there is a further layer of connective tissue that surrounds the smooth muscle. This connective tissue, which is mostly made up of collagen, contains nerves that supply the smooth muscular layer. The connective tissue surrounding larger vessels also contains capillaries to bring nutrients to the tissue. Capillaries, the smallest blood vessels, are made up of a single layer of endothelium and a small amount of connective tissue.
Arteries and Arterioles

Figure 8: The structure of an artery wall.
The arteries carry blood away from the heart. As shown in Figure 8, arteries have thick walls that have three major layers; an inner endothelial layer, a middle layer of smooth muscle, and an outer layer of stretchy connective tissue (mostly collagen). The elastic qualities of artery walls allow them to carry pressurized blood from the heart while maintaining blood pressure.
The aorta is the largest artery in the body. It receives blood directly from the left ventricle of the heart through the aortic valve. The aorta branches, into smaller arteries and these arteries branch in turn, becoming smaller in diameter, down to arterioles. The arterioles supply the capillaries that carry nutrients to the body’s cells and tissues. The aorta is an elastic artery. When the left ventricle contracts to force blood into the aorta, it expands. This stretching gives the potential energy that will help maintain blood pressure during diastole when the aorta contracts passively.
An arteriole is a small-diameter blood vessel that branches out from an artery and leads to capillaries. Arterioles have thin muscular walls, composed of one or two layers of smooth muscle, and are the primary site of vascular resistance. Vascular resistance is the resistance to flow that blood must overcome to be pumped through your circulatory system. Increasing vascular resistance is one way your body can increase blood pressure.
Veins and Venuoles
Veins return deoxygenated blood to the heart. The thick, outer layer of a vein is made up of collagen-containing connective tissue, shown in Figure 9. The connective tissue is wrapped around bands of smooth muscle while the interior is lined with endothelium. Most veins have one-way flaps called valves, shown in in Figure 10, that prevent blood from flowing backward and pooling in the legs, feet, arms or hands due to the pull of gravity. The location of veins can vary from person to person.

Figure 9: Internal structure of a vein.

Figure 10: Valves found in veins prevent the blood from flowing backward and pooling in the lowest parts of the body, such as the legs and feet.
A venule is a small blood vessel that allows deoxygenated blood to return from the capillary beds to the larger blood vessels called veins. Venules have three layers: an inner endothelium composed of squamous epithelial cells that act as a membrane, a middle layer of muscle and elastic tissue, and an outer layer of fibrous connective tissue. The middle layer is poorly developed so that venules have thinner walls than arterioles.
Capillaries
Capillaries are the smallest of a body’s blood vessels, measuring 5-10 \(\mu\)m in diameter. Their size is shown in relation to body cells in Figure 11. Capillaries connect arterioles and venules, and they are important for the exchange of oxygen, carbon dioxide, and other substances between blood and body cells.

Figure 11: The structure of capillaries. Note their size in comparison to the cells around them.
The walls of capillaries are made of only a single layer of endothelial cells. This layer is so thin that molecules such as oxygen, water and lipids can pass through them by diffusion and enter the body tissues. Waste products such as carbon dioxide and urea can diffuse back into the blood to be carried away for removal from the body. Capillaries are so small the blood cells need to pass through it in a single file line. A capillary bed is the network of capillaries supplying an organ. The more metabolically active a tissue or organ is, the more capillaries it needs to get nutrients and oxygen.
Blood vessels are roughly grouped as arterial and venous. This grouping is determined by whether the blood in the vessel is flowing away from (arterial) or toward (venous) the heart. In general the term arterial blood is used to describe blood high in oxygen, although the pulmonary arteries carry deoxygenated blood and blood flowing in the pulmonary vein is rich in oxygen.
Roles of Blood Vessels
Blood vessels are not involved in regulating the transport of blood, the endocrine and nervous systems do that. However, arteries and veins can regulate their inner diameter by contraction of the smooth muscle layer. This widening or narrowing of the blood vessels changes the blood flow to the organs of the body. This process is controlled by the autonomic nervous system; it is not controlled consciously.
Vasodilation is a process by which blood vessels in the body become wider due to the relaxation of the smooth muscle in the vessel wall. This reduces blood pressure since there is more room for the blood to move through the vessel. Endothelium of blood vessels uses nitric oxide to signal the surrounding smooth muscle to relax, which dilates the artery and increasing blood flow. Nitric dioxide is a vasodilator.
Vasoconstriction is the constriction of blood vessels (narrowing, becoming smaller in cross-sectional area) by contracting the vascular smooth muscle in the vessel walls. Vasoconstriction is controlled by substances such as some hormones and neurotransmitters, which are called vasoconstrictors. For example, the “fight or flight” hormone epinephrine is a vasoconstrictor that is released by the adrenal glands.
Permeability of the endothelium is important for the release of nutrients to the tissue. Permeability is the ability of a membrane to allow certain molecules and ions to pass through it by diffusion. Permeability of the endothelium increases during an immune response, which allows white blood cells and other substances to get to the site of injury or irritation.
Oxygen, which is bound to hemoglobin in red blood cells for transport through the body, is the most critical nutrient carried by the blood. In all arteries apart from the pulmonary artery, hemoglobin is highly saturated (95-100%) with oxygen. In all veins apart from the pulmonary vein, the hemoglobin is desaturated at about 70%. (The values are reversed in the pulmonary circulation.)
Blood Vessels and Blood Pressure
Blood pressure refers to the force exerted by circulating blood on the walls of blood vessels. The pressure of the circulating blood gradually decreases as blood moves from the arteries, arterioles, capillaries, and veins. The term ”blood pressure” generally refers to arterial pressure, which is the pressure in the larger arteries that take blood away from the heart.
Arterial pressure results from the force that is applied to blood by the contracting heart, where the blood “presses” against the walls of the arteries.
The systolic arterial pressure is defined as the peak pressure in the arteries, which occurs near the beginning of the cardiac cycle; the diastolic arterial pressure is the lowest pressure (at the resting phase of the cardiac cycle).
Arterial pressure is most commonly measured by a sphygmomanometer, shown in Figure 12. The height of a column of mercury indicates the pressure of the circulating blood. Although many modern blood pressure devices no longer use mercury, values are still universally reported in millimeters of mercury (mmHg).

Figure 12: The new and the “classic” ways to measure blood pressure. A digital sphygmomanometer, shown on the left, runs on electricity or batteries and measure blood pressure automatically. The cuff, which you can see behind the digital readout, is wrapped around the upper arm, just like the cuff of the older devices. The cuff then inflates automatically and measures blood pressure as the cuff deflates. The older, mechanical sphygmomanometer with a cuff and pressure reader and stethoscope is shown at right. The cuff is inflated and deflated manually while a medical technician listens for related changes in the sound of blood moving through arteries in the arm.
Blood Pressure Ranges
In the U.S., the healthy ranges for arterial pressure are:
• Systolic: less than 120 mm Hg
• Diastolic: less than 80 mm Hg
Blood pressure is usually written as systolic/diastolic mm Hg; for example, a reading of 120/80 mm Hg, is said as ”one twenty over eighty.” These measures of arterial pressure are not static, but go through natural variations from one heartbeat to another and throughout the day (in a circadian rhythm). Factors such as age, gender and race influence blood pressure values. Pressure also varies with exercise, emotional reactions, sleep, stress, nutritional factors, drugs, or disease.
Studies have shown that people whose systolic pressure is around 115 mm Hg rather than 120 mmHg have fewer health problems. Clinical trials have shown that people who have arterial pressures at the low end of these ranges have much better long term cardiovascular health for this reason some researchers say that 115/75 mm Hg should be the ideal measurement.
Hypertension is a condition in which a person’s blood pressure is chronically high. Hypertension is said to be present when a person’s systolic blood pressure is always 140 mm Hg or higher, and/or their diastolic blood pressure is always 90 mm Hg or higher. Blood pressure readings between 120/80 mmHg and 139/89 mmHg are called prehypertension. Prehypertension is not a disease category; rather, it is a way to identify people who are at high risk of developing hypertension.
Arterioles and Blood Pressure
Arterioles have the greatest collective influence on both local blood flow and on overall blood pressure. They are the primary ”adjustable nozzles” in the blood system, across which the greatest pressure drop occurs. The combination of heart output (cardiac output) and systemic vascular resistance, which refers to the collective resistance of all of the body’s arterioles, are the principal determinants of arterial blood pressure at any given moment.
Pulmonary and Systemic Circulations
The double circulatory system of blood flow refers to the separate systems of pulmonary circulation and the systemic circulation in amphibians, birds and mammals, including humans. The adult human heart consists of two separated pumps, the right side which pumps deoxygenated blood into the pulmonary circulation, and the left side which pumps oxygenated blood into the systemic circulation. Blood in one circuit has to go through the heart to enter the other circuit, as shown in Figure 13.

Figure 13: The double circulatory system. Blood in one circuit has to go through the heart to enter the other circuit. The heart-to-lungs-to heart portion is the pulmonary circulation, and the heart-to-body-to-heart portion is the systemic circulation.
Pulmonary Circuit
The pulmonary circulation is the portion of the cardiovascular system which carries oxygen-poor (deoxygenated) blood away from the heart, to the lungs, and returns oxygenated blood back to the heart. As shown in Figure 14, deoxygenated blood from the body leaves the right ventricle through the pulmonary arteries, which carry the blood to each lung. The pulmonary arteries are the only arteries that carry deoxygenated blood. In the lungs, red blood cells release carbon dioxide and pick up oxygen during respiration. The oxygenated blood then leaves the lungs through the pulmonary veins, which return it to the left side of the heart, and complete the pulmonary cycle. The oxygenated blood is then distributed to the body through the systemic circulation before returning again to the pulmonary circulation.

Figure 14: Pulmonary circulation. The pulmonary arteries carry oxygen-poor blood from the right ventricle to the lungs, and the pulmonary veins return oxygenated blood to the left side of the heart. This “loop” is called the pulmonary cycle.
The pulmonary circulation was first discovered by a Syrian physician, Ibn al-Nafis, in 1242. However, credit for the first description of blood circulation is given to an English medical doctor William Harvey, who in 1616 described in detail the pulmonary and systemic circulation systems.
Systemic Circulation
The systemic circulation is the portion of the cardiovascular system which carries oxygenated blood away from the heart, to the body, and returns deoxygenated blood back to the heart. Oxygenated blood from the lungs leaves the left ventricle through the aorta, from where it is distributed to the body’s organs and tissues, which absorb the oxygen, through a complex network of arteries, arterioles, and capillaries. The deoxygenated blood is then collected by venules, from where it flows first into veins, and then into the inferior and superior venae cavae, which return it to the right heart, completing the systemic cycle, shown in Figure 15. The blood is then re-oxygenated through the pulmonary circulation before returning again to the systemic circulation.

Figure 15: The systemic circulation. The systemic circulation brings oxygenated blood to the body cells and tissues and transports cellular wastes. It is also responsible for temperature regulation and transport of hormones and other substances around the body.
Just like every other organ in the body, the heart needs its own blood supply, which it gets through the coronary circulation. Although blood fills the chambers of the heart, the heart muscle tissue is so thick that it needs blood vessels to deliver oxygen and nutrients deep within it. The vessels that deliver oxygen-rich blood to the heart muscle are called coronary arteries, they branch directly from the aorta, just above the heart, shown in Figure 16. The vessels that remove the deoxygenated blood from the heart muscle are known as cardiac veins.

Figure 16: This side view (lateral view), of the heart shows how the coronary arteries (in red) branch directly from the aorta to bring oxygen and nutrients into the heart muscle.
Portal Venous System
A portal venous system occurs when a capillary bed drains into another capillary bed through veins. They are relatively uncommon as the majority of capillary beds drain into the heart, not into another capillary bed. Portal venous systems are considered venous because the blood vessels that join the two capillary beds are either veins or venules.
An example of a portal venous system is the blood vessel network between the digestive tract and the liver. The hepatic portal system is responsible for directing blood from parts of the gastrointestinal tract to the liver. Nutrients that have been absorbed into the blood from the small intestine are taken to the liver for processing before being sent to the heart. The term, ”portal venous system” often refers to the hepatic portal system.
Lymphatic System
The lymphatic system, shown in Figure 17, is a complex network of lymph nodes, lymph ducts, lymphatic tissues, lymph capillaries and lymph vessels that extend the length of the body. It serves as a conduit for a fluid called lymph. The lymphatic system is often called the secondary circulatory system.

Figure 17: Lymphatic system.
The lymphatic system has three related functions:
• The removal of excess fluids from body tissues.
• The absorption of fats, also known as fatty acids or lipids, and transport of fats to the cardiovascular system.
• The production of certain types of white blood cells, which aid in the body’s immune response.
Lymph originates as blood plasma that leaks from the capillaries of the cardiovascular system. This blood plasma fills the space between individual cells of tissue where it becomes part of the interstitial fluid. Plasma is forced out of the capillaries and forced back in due to interactions of hydrostatic pressure. While out of the blood capillaries, the plasma increases the volume of the interstitial fluid. Most of the interstitial fluid is returned to the capillaries by osmosis. The excess interstitial fluid is collected by the lymphatic system by diffusion into lymph capillaries, and is processed by lymph nodes before to being returned to the circulatory system. Once within the lymphatic system the fluid is called lymph, and has almost the same composition as the original interstitial fluid.
Fatty acids, also known as fats or lipids, are transported through the cardiovascular system differently than other nutrients, such as proteins and sugars. Lipids are absorbed by cells in the villi of the small intestine where they form a complex with protein molecules. These lipo-proteins are called chylomicrons. The chylomicrons are transported via the lymphatic system and eventually rejoin the bloodstream to be processed by the liver.
The lymphatic system is a major component of the immune system. The lymphatic system has many lymph nodes. Lymph nodes are filters or traps for foreign particles and contain white blood cells. Human lymph nodes are bean-shaped and range in size from a few millimeters to about 1 to 2 cm. White blood cells are located within honeycomb structures of the lymph nodes. Lymph that moves through the lymph nodes is filtered so that microorganisms and tissue debris are removed. Lymph nodes swell and feel sore when the body is infected due to the increased production of white blood cells.
The spleen and tonsils are large lymphoid organs that serve similar functions to lymph nodes, though the spleen filters blood cells rather than bacteria or viruses.
Lymphatic Circulation
Unlike the blood system, the lymphatic system is not closed and has no central pump. Lymph movement occurs slowly with low pressure due to peristalsis, valves, and the squeezing action of skeletal muscles. Lymph travels through lymph vessels that are similar to capillaries and veins. Lymph moves in one direction only, due to valves in lymph vessels that are similar to the valves found in veins, shown in Figure 18. The movement of lymph depends on the movement of skeletal muscles to squeezing the lymph through them, especially near the joints. Rhythmic contraction of the vessel walls through movements may also help draw fluid into the small lymphatic capillaries. The lymph is then transported to progressively larger lymphatic vessels that drain into the circulatory system at the right and left subclavian veins.

Figure 18: The movement of lymph from the interstitial fluid into the lymphatic vessels. Lymph moves in only one direction through the blood vessels.
Homeostatic Imbalance of the Lymphatic System
In the disease known as elephantiasis, shown in Figure 19, infection of the lymphatic vessels cause a thickening of the skin and enlargement of the underlying tissues, especially in the legs and genitals. It is most commonly caused by infection by parasitic roundworms.

Figure 19: Over a billion people are at risk for infection by filarial nematodes, the parasites that cause elephantiasis.
Lymphedema also causes abnormal swelling, especially in the arms and legs (though the face, neck, and abdomen can also be affected). It occurs if the lymphatic system is damaged, or underdeveloped in some way. An estimated 170 million suffer with the disorder.
Lymphoma, or lymphatic cancer, is cancer of the lymphatic system. According to the American Cancer Society, in 2007, lymphoma accounted for 4 percent of new cancer cases amongst men and women in the United States. In lymphoma, cells of the lymphatic system grow abnormally. They divide too rapidly and grow without any order or control. Because lymphatic tissue is present in many parts of the body, lymphoma can start almost anywhere. Lymphoma may occur in a single lymph node, a group of lymph nodes, or, sometimes, in other parts of the lymphatic system such as the bone marrow and spleen.
Homeostatic Imbalances of the Cardiovascular System
Cardiovascular disease (CVD) refers to any disease that affects the cardiovascular system, but it is usually used to refer to diseases related to atherosclerosis, which is a chronic inflammatory response in the walls of arteries that causes a swelling and buildup of materials called plaque. Plaque is made of cell debris, cholesterol, fatty acids, calcium, and fibrous connective tissue that build up around an area of inflammation. As a plaque grows it stiffens and narrows the artery, which reduces the flow of blood through the artery, shown in Figure 20.

Figure 20: Atherosclerosis is sometimes referred to as hardening of the arteries.
Atherosclerosis
Atherosclerosis normally begins in later childhood, and is usually found in most major arteries. It does not usually have any early symptoms. Causes of atherosclerosis include a high-fat diet, high cholesterol, smoking, obesity, and diabetes. Atherosclerosis becomes a threat to health when the plaque buildup interferes with the blood circulation in the heart (coronary circulation) or the brain (cerebral circulation). A blockage in the coronary circulation, can lead to a heart attack, and blockage of the cerebral circulation (leading to, or within the brain) can lead to a stroke. According to the American Heart Association, atherosclerosis is a leading cause of CVD.
Coronary Heart Disease
Cardiac muscle cells are fed by the coronary arteries. Blocked flow in a coronary artery can result in oxygen starvation and death of heart muscle. Coronary heart disease is the end result of the buildup of plaques within the walls of the coronary arteries, shown in Figure 21. Most individuals with coronary heart disease have no symptoms for many years until the first sign, often a heart attack, happens.

Figure 21: Autopsy specimen of an artery has been opened lengthwise to show the inside (lumen) which is completely blocked by many plaques.
A symptom of coronary heart disease is chest pain. Occasional chest pain, called angina pectoralis (or angina) can happen during times of stress or physical exertion. The pain of angina means the heart muscle fibers need more oxygen than they are getting.
A heart attack, also called a myocardial infarction (MI), occurs when the blood supply to a part of the heart is blocked, as shown in Figure 22.22. A heart attack can occur from the buildup and blockage of a coronary artery by plaque, or it can be caused by a small piece of plaque that breaks away when a larger plaque breaks apart. This piece of free-floating plaque, called an embolus, can get stuck in a coronary blood vessel, causing a blockage or embolism. Cardiac muscle fibers that are starved of oxygen for more than five minutes will die, and because they do not divide, dead cardiac muscle cells cannot be replaced. Coronary heart disease is the leading causes of death of adults in the United States.

Figure 22: Diagram of a heart attack (myocardial infarction). The blood supply to the lower part of the heart is stopped after a blockage of the lower portion of the left coronary artery (LCA).
Stroke
Since atherosclerosis is a body wide process, similar events can also occur in the arteries to other parts of the body, including the brain. A stroke is a loss of brain function due to a stoppage of the blood supply to the brain. It can be caused by a blot clot (thrombosis), a free-floating object that gets caught in a blood vessel (embolism), or by bleeding (hemorrhage).
Risk factors for stroke include advanced age, high blood pressure, previous stroke, diabetes, high cholesterol, and cigarette smoking. Reduction of blood pressure is the most important modifiable risk factor of stroke; however many other risk factors, such as quitting tobacco smoking, are also important.
Preventing Cardiovascular Diseases
There are many risk factors which are associated with various forms of cardiovascular disease, some of these you cannot control, but many you can control.
Non-controllable risk factors include:
• Age: The older a person is, the greater their chance of developing a cardiovascular disease.
• Gender: Men under age 64 are much more likely to die of coronary heart disease than women, although the gender difference declines with age.
• Genetics: Family history of cardiovascular disease affects a person’s chance of developing heart disease.
Controllable risk factors include:
• Tobacco Smoking: Giving up smoking is the single most effective way of reducing risk of heart disease.
• Diabetes: Having diabetes can cause metabolic changes (such as high cholesterol levels) which in themselves are risk factors.
• High cholesterol levels: High amounts of low density lipids (LDLs) in the blood, also called ”bad cholesterol”, are a significant risk factor.
• Obesity: Being obese, especially if the fat is deposited mostly in the torso, rather than the hips and thighs, increases risk significantly.
• High blood pressure: Hypertension can cause atherosclerosis.
• Lack of physical activity: Aerobic activities, including walking and vacuuming, that are done for 60 minutes a day, five days a week, help keep the heart healthy.
• Poor eating habits: Eating mostly foods that are nutrient poor (do not have many nutrients other than fat or carbohydrate) leads to high cholesterol levels and weight gain, among other things.
Although there are uncontrollable risk factors involved in CVD, a person whose family has a history of CVD is not destined to develop heart disease. There are many things such a person can do to help prevent CVD, even when predisposed to a disease. A person who is physically active every day, eats healthfully, and avoids tobacco can lower their chances of developing the disease.
Although men have a higher rate of cardiovascular disease than women, it is also the number one health problem for women in industrialized countries. After menopause, the risk for women is almost equal to that of men.
Cardiovascular Disease Awareness
Cardiovascular diseases are called ”lifestyle diseases” because they are caused mostly by everyday choices that people make, such as what to eat for dinner, or what to do during their free time. For example, watching TV with your dog does not involve much moving around so it does not exercise the body, whereas bringing the dog for a walk outside exercises both of you. Decisions that you make today and everyday will affect your cardiovascular health many years from now, such as those shown in Figure 23.

Figure 23: Limiting sedentary activities such as watching TV, and making more time for walking, hiking, cycling, or running will help develop a healthy heart.
Many studies have shown that plaque buildup starts in early adolescence. However, teens are more concerned about risks such as HIV, accidents, and cancer than cardiovascular disease. One in three people will die from complications due to atherosclerosis. For this reason there is an emphasis on the prevention of CVD through risk reduction. For example, healthy eating, regular physical activity, and avoidance of smoking can greatly decrease a person’s chance of developing a CVD.
Congenital Hearth Defects
A congenital heart defect is a problem with the structure of the heart that is present at birth. Such heart defects are the most common type of major birth defect. Most heart defects either obstruct blood flow in the heart or vessels near it, or cause blood to flow through the heart in an abnormal pattern, although other defects affecting heart rhythm can also occur.
Treatment for a defect can include medicines, surgery, and other medical procedures and heart transplants. The treatment depends on the type and severity of the defect and the child’s age, size and general health. Also, certain mild defects that some children are born with are repaired over time by the body.
Images courtesy of:
Sansculotte. http://commons.wikimedia.org/wiki/Image:Grafik_blutkreislauf.jpg. CC-BY-SA-2.5.
http://training.seer.cancer.gov/anatomy/cardiovascular/heart/structure.html. Public Domain.
http://commons.wikimedia.org/wiki/Image:Mediastinum_anatomy.jpg. CC-BY-2.5.
http://en.wikipedia.org/wiki/Image:Bundleofhis.png. Public Domain.
http://en.wikipedia.org/wiki/Image:Purkinje_fibers.jpg. CC-BY-SA.
http://en.wikipedia.org/wiki/Image:Heart_diastole.png. GNU-FDL.
http://en.wikipedia.org/wiki/Image:Veincrosssection.png. Public Domain, GNU-FDL.
http://en.wikipedia.org/wiki/Image:Illu_capillary.jpg. Public Domain.
http://commons.wikimedia.org/wiki/Image:Sphygmomanometer.jpg. GNU-FDL, Public Domain.
http://en.wikipedia.org/wiki/Image:Double_circulatory_system.jpg. Public Domain.
http://en.wikipedia.org/wiki/Image:Illu_pulmonary_circuit.jpg. Public Domain.
http://training.seer.cancer.gov/anatomy/cardiovascular/blood/pathways.html. Public Domain.
http://commons.wikimedia.org/wiki/Image:Heart_left_lateral_coronaries_diagram.svg. CC-BY-2.5.
USFG. http://commons.wikimedia.org/wiki/Image:Illu_lymph_capillary.png. Public Domain.
Dr. Steven A. Williams. http://commons.wikimedia.org/wiki/Image:Elephantiasis.png. CC-BY-2.5.
http://commons.wikimedia.org/wiki/Image:Heart_coronary_artery_lesion.jpg. CC-BY-2.5.
J. Heuser. http://en.wikipedia.org/wiki/Image:AMI_scheme.png.
http://www.flickr.com/photos/johnjoh/349825408/. CC-BY-SA, CC-BY-SA.