The Skeletal System
Article objectives
How important is your skeleton? Can you imagine what you would look like without it?
You would be a wobbly pile of muscle and internal organs, maybe a little similar to the slug in Figure 1. Not that you would really be able to see yourself anyway, due to the folds of skin that would droop over your eyes because of your lack of skull bones. You could push the skin out of the way, if you could only move your arms!

Figure 1: Banana slugs (Ariolimax spp.), unlike you, can live just fine without a bony skeleton. They can do so because they are relatively small and their food source (vegetation) is plentiful and tends not to run away from them. Slugs move by causing a wave-like motion in their foot, (the ventral (bottom) area of the slug that is in contact with the ground). Slugs and other gastropods also live in environments very different to humans’ environments. Just think of how a bony skeleton would be of limited use to a slug whose lifetime is spent under a log munching on rotting leaf litter.
The Skeleton
Humans are vertebrates, which are animals that have a vertebral column, or backbone. Invertebrates, like the banana slug in Figure 1, do not have a vertebral column, and use a different mechanism than vertebrates to move about. The sturdy internal framework of bones and cartilage that is found inside vertebrates, including humans, is called an endoskeleton. The adult human skeleton consists of approximately 206 bones, some of which are named in Figure 2. Cartilage, another component of the skeleton can also be seen in Figure 2. Cartilage is a type of dense connective tissue that is made of tough protein fibers. The function of cartilage in the adult skeleton is to provide smooth surfaces for the movement of bones at a joint. A ligament is a band of tough, fibrous tissue that connects bones together. Ligaments are not very elastic and some even prevent the movement of certain bones.

Figure 2: The skeleton is the bone and cartilage scaffolding that supports the body, and allows it to move. Bones act as attachment points for the muscles and tendons that move the body. Bones are also important for protection. For example, your skull bones (cranium) protect your brain, and your ribcage protects your heart and lungs. Cartilage is the lightgray material that is found between some of the bones and also between the ribcage and sternum.
The skeletons of babies and children have many more bones and more cartilage than adults have. As a child grows, these “extra” bones, such as the bones of the skull (cranium), and the sacrum (tailbone) fuse together, and cartilage gradually hardens to become bone tissue.
The bones of the skeleton can be grouped in two divisions: the axial skeleton and appendicular skeleton. The axial skeleton includes the bones of the head, vertebral column, ribs and sternum, in the left portion of Figure 3. There are 80 bones in the axial skeleton. The appendicular skeleton includes the bones of the limbs (arms and legs) along with the scapula and the pelvis, and is shown at right in Figure 3. There are approximately 126 bones in the appendicular skeleton. Limbs are connected to the rest of the skeleton by collections of bones called girdles. The pectoral girdle consists of the clavicle (collar bone) and scapula (shoulder blade). The pelvic girdle consists of two pelvic bones (hipbones) that form the pelvic girdle. The vertebral column attaches to the top of the pelvis; the femur of each leg attaches to the bottom. The humerus is joined to the pectoral girdle at a joint and is held in place by muscles and ligaments.

Figure 3: The two divisions of the human skeleton. The bones of the axial skeleton are blue, and the bones of the appendicular skeleton are pink.
Function and Structure of Bones
Many people think of bones as dry, dead, and brittle, which is what you might think if you saw a preserved skeleton in a museum. The association of bones with death is illustrated by the sweets shown in Figure 4. This is a common association because the calcium-rich bone tissue of a vertebrate is the last to decompose after the organism dies. However, the bones in your body are very much alive. They contain many tough protein fibers, are crisscrossed by blood vessels, and certain parts of your bones are metabolically active. Preserved laboratory skeletons are cleaned with chemicals that remove all organic matter from the bones, which leaves only the calcium-rich mineralized (hardened) bone tissue behind.

Figure 4: Sugar skulls made to celebrate Dia de Los Muertos (Day of the Dead), a time (the 1st and 2nd of November) during which the people of Mexico and some Latin American countries celebrate and honor the lives of the deceased, and celebrate the continuation of life.
Functions of Bones
Your skeletal system is important for the proper functioning of your body. In addition to giving shape and form to the body, bones have many important functions.
The main functions of bones are:
• Structural Support of the Body: The skeleton supports the body against the pull of gravity. The large bones of the lower limbs support the trunk when standing.
• Protection of Internal Organs: The skeleton provides a rigid frame work that supports and protects the soft organs of the body. The fused bones of the cranium surround the brain to make it less vulnerable to injury. Vertebrae surround and protect the spinal cord and bones of the rib cage help protect the heart and lungs.
• Attachment of the Muscles: The skeleton provides attachment surfaces for muscles and tendons which together enable movement of the body.
• Movement of the Body: Bones work together with muscles as simple mechanical lever systems to produce body movement.
• Production of Blood Cells: The formation of blood cells takes place mostly in the interior (marrow) of certain types of bones.
• Storage of Minerals: Bones contain more calcium than any other organ in the form of calcium salts such as calcium phosphate. Calcium is released by the bones when blood levels of calcium drop too low. Phosphorus is also stored in bones.
Structure of Bones
Although bones vary greatly in size and shape, they all have certain structural similarities. Bones are organs.Recall that organs are made up of two or more types of tissues. The two main types of bone tissue are compact bone and spongy bone. Compact bone makes up the dense outer layer of bones. Spongy bone is lighter and less dense than compact bone, and is found toward the center of the bone. Periosteum (from peri = around, osteo = bone),is the tough, shiny, white membrane that covers all surfaces of bones except at the joint surfaces. Periosteum is composed of a layer of fibrous connective tissue and a layer of bone forming cells. These structures can be seen in Figure 5.

Figure 5: Structure of a typical bone. The components that make up bones can be seen here. Compact bone is the dense material that makes up the outer ring of the bone. Most bones of the limbs are long bones, including the bones of the fingers. The classification of “long bone” refers to the shape of the bone rather than to the size.
Compact Bone
Just below the periosteum is the hard layer of compact bone tissue. It is so called due to its high density, and it accounts for about 80% of the total bone mass of an adult skeleton. Compact bone is extremely hard, and is made up of many cylinder-shaped units called osteons, or Haversian systems. Osteons act like strong pillars within the bone to give the bone strength and allow it to bear the weight of the attached muscles and withstand the stresses of movement. As you can see in Figure 6, osteons are made up of rings of calcium salts and collagen fibers, called bone matrix. Bone matrix is a mixture of calcium salts, such as calcium phosphate and calcium hydroxide, and collagen fibers (a type of protein) which form hollow tubes that look similar to the rings on a tree. Each of these matrix tubes is a lamella, which means “thin plate” (plural: lamellae). The calcium salts form crystals that give bones great strength, but the crystals do not bend easily, and tend to shatter if stressed. Collagen fibers are tough and flexible. All collagen fibers within a single lamella are lined up in the same direction, which gives each lamella great strength. Overall, the protein-calcium crystal combination in the matrix allows bones to bend and twist without breaking easily. The collagen fibers also act as a scaffold for the laying down of new calcium salts.

Figure 6: The internal structure of a bone. Both compact and spongy bone can be seen.
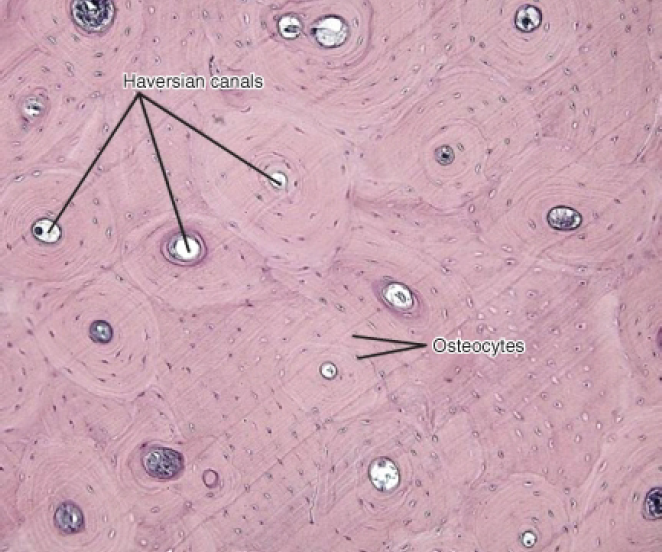
Figure 7: The location of Haversian canals and osteocytes in osteons of compact bone.
In the center of each osteon is a Haversian canal. The canal serves as a passageway for blood vessels and nerves. Within each osteon, many bone cells called osteocytes are located. Osteocytes are found in little pockets called lacunae that are sandwiched between layers of bone matrix. You can see lamellae and osteocytes in their lacunae in Figure 7. Osteocytes are responsible for monitoring the protein and mineral content of the bone and they direct the release of calcium into the blood and the uptake up of calcium salts into the bone. Other bone cells, called osteoblasts secrete the organic content of matrix, and are responsible for the growth of new bone. Osteoblasts are found near the surface of bones. Osteoclasts are bone cells that remove calcium salts from bone matrix. In the meantime, Table 1 describes some of the different structures and functions of bones.
Table 1: Pituitary Hormones
| Function | Location | |
|---|---|---|
| Osteons (also known as Haversion systems) | Act like pillars to give bone strength | Compact bone |
| Bone Matrix | A mixture of calcium salts and collagen fibers which form hollow tubes that look similar to the rings on a tree | Compact bone, spongy bone |
| Lamella | Layers of bone matrix in which collagen fibers point in the opposite direction to the fibers of the lamellae to each side, offers great strength and flexibility | Are the “tree rings” of osteons |
| Lacunae | Location of osteocytes | Between lamellae of bone matrix |
| Osteocytes | Monitor the protein and mineral content of bone and direct the release of calcium into the blood; control the uptake up of calcium salts into the bone | Within lacunae of osteons |
| Osteoblasts | Bone-forming cell; secretes organic part of matrix (collagen) | Found near the surface of bones |
| Osteoclasts | Responsible for the breakdown of matrix and release of calcium salts into the blood. | Bone surfaces |
| Chondrocyte | Cartilage-forming cell | |
| Periosteum | Contains pain receptors and is sensitive to pressure or stress; provides nourishment through a good the blood supply; provides an attachment for muscles and tendons | |
| Collagen fibers | Tough protein fibers that give bones flexibility and prevent shattering. | |
| Calcium salts | Form crystals that give bones great strength. |
Spongy Bone
Spongy bone occurs at the ends of long bones and is less dense than compact bone. The term “spongy” refers only to the appearance of the bone, as spongy bone is quite strong. The lamellae of spongy bone form an open, porous network of bony branches, or beams called trabiculae, that give the bone strength and make the bone lighter. It also allows room for blood vessels and bone marrow. Spongy bone does not have osteons, instead nutrients reach the osteocytes of spongy bone by diffusion through tiny openings in the surface of the spongy bone. Spongy bone makes up the bulk of the interior of most bones, including the vertebrae.
Bone Marrow
Many bones also contain a soft connective tissue called bone marrow. There are two types of bone marrow: red marrow and yellow marrow. Red marrow produces red blood cells, platelets, and most of the white blood cells for the body. Yellow marrow produces white blood cells. The color of yellow marrow is due to the high number of fat cells it contains. Both types of bone marrow contain numerous blood vessels and capillaries. In newborns, bones contain only red marrow. As the child ages, red marrow is mostly replaced by yellow marrow. In adults, red marrow is mostly found in the flat bones of the skull, the ribs, the vertebrae and pelvic bones. It is also found between the spongy bone at the very top of the femur and the humerus.
Periosteum
The outer surfaces of bones—except where they make contact with other bones at joints—are covered by periosteum. Periosteum has a tough, external fibrous layer, and an internal layer that contains osteoblasts (the bone-growing cells). The periosteum is richly supplied with blood, lymph and nociceptors, which make it very sensitive to manipulation (recall that nociceptors are pain receptors that are also found in the skin and skeletal muscle). Periosteum provides nourishment to the bone through a rich blood supply. The periosteum is connected to the bone by strong collagen fibers called Sharpey’s fibres, which extend into the outer lamellae of the compact bone.
Bone Shapes
The four main types of bones are long, short, flat, and irregular. The classification of a bone as being long, short, flat, or irregular is based on the shape of the bone rather than the size of the bone. For example, both small and large bones can be classified as long bones. There are also some bones that are embedded in tendons, these bones tend to be oval-shaped and are called sesamoid bones.
• Long Bones: Bones that are longer than they are wide are called long bones. They consist of a long shaft with two bulky ends. Long bones are primarily made up of compact bone but may also have a large amount of spongy bone at both ends. Long bones include bones of the thigh (femur), leg (tibia and fibula), arm (humerus), forearm (ulna and radius), and fingers (phalanges). The classification refers to shape rather than the size.
• Short Bones: Short bones are roughly cube-shaped, and have only a thin layer of compact bone surrounding a spongy interior. The bones of the wrist (carpals) and ankle (tarsals) are short bones, as are the sesamoid bones (see below).
• Sesamoid Bones: Sesamoid bones are embedded in tendons. Since they act to hold the tendon further away from the joint, the angle of the tendon is increased and thus the force of the muscle is increased. An example of a sesamoid bone is the patella (kneecap).
• Flat Bones: Flat bones are thin and generally curved, with two parallel layers of compact bones sandwiching a layer of spongy bone. Most of the bones of the skull (cranium) are flat bones, as is the sternum (breastbone).
• Irregular Bones: Irregular bones are bones that do not fit into the above categories. They consist of thin layers of compact bone surrounding a spongy interior. As implied by the name, their shapes are irregular and complicated. The vertebrae and pelvis are irregular bones.
All bones have surface markings and characteristics that make a specific bone unique. There are holes, depressions, smooth facets, lines, projections and other markings. These usually represent passageways for vessels and nerves, points of articulation with other bones or points of attachment for tendons and ligaments.
Cellular Structure of Bone
When blood calcium levels decrease below normal, calcium is released from the bones so that there will be an adequate supply for metabolic needs. When blood calcium levels are increased, the excess calcium is stored in the bone matrix. The dynamic process of releasing and storing calcium goes on almost continuously, and is carried out by different bone cells.
There are several types of bone cells.
• Osteoblasts are bone-forming cells which are located on the inner and outer surfaces of bones. They make a collagen-rich protein mixture (called osteoid), which mineralizes to become bone matrix. Osteoblasts are immature bone cells. Osteoblasts that become trapped in the bone matrix differentiate into osteocytes. The osteocytes stop making osteoid and instead direct the release of calcium from the bones and the uptake of calcium from the blood.
• Osteocytes originate from osteoblasts which have migrated into and become trapped and surrounded by bone matrix which they themselves produce. The spaces which they occupy are known as lacunae. Osteocytes are star-shaped, and they have many processes which reach out to meet osteoblasts probably for the purposes of communication. Their functions include matrix maintenance and calcium homeostasis. They are mature bone cells. Refer to Figure 7 for the location of osteocytes.
• Osteoclasts are the cells responsible for bone resorption, which is the remodeling of bone to reduce its volume (see below). Osteoclasts are large cells with many nuclei, and are located on bone surfaces. They secrete acids which dissolve the calcium salts of the matrix, releasing them into the blood stream. This causes the calcium and phosphate concentration of the blood to increase. Osteoclasts constantly remove minerals from the bone, and osteoblasts constantly produce matrix that binds minerals into the bone, so both of these cells are important in calcium homeostasis.
Bone Cells and Calcium Homeostasis
Remodeling or bone turnover is the process of resorption of minerals followed by replacement by bone matrix which causes little overall change in the shape of the bone. This process occurs throughout a person’s life. Osteoblasts and osteoclasts communicate with each other for this purpose. The purpose of remodeling is to regulate calcium homeostasis, repair micro-damaged bones (from everyday stress), and also to shape the skeleton during skeletal growth.
The process of bone resorption by the osteoclasts releases stored calcium into the systemic circulation and is an important process in regulating calcium balance. As bone formation actively fixes circulating calcium in its mineral form, removing it from the bloodstream, resorption actively unfixes it thereby increasing circulating calcium levels. These processes occur in tandem at site-specific locations.
Development of Bones
The terms osteogenesis and ossification are often used to indicate the process of bone formation. The skeleton begins to form early in fetal development. By the end of the eighth week after conception, the skeletal pattern is formed by cartilage and connective tissue membranes. At this point, ossification begins.
Early in fetal development, the skeleton is made of cartilage. Cartilage is a type of dense connective tissue that is composed of collagen fibers and/or elastin fibers, and cells called chondrocytes which are all set in a gel-like substance called matrix. Cartilage does not contain any blood vessels so nutrients diffuse through the matrix to the chondrocytes. Cartilage serves several functions, including providing a framework upon which bone deposition can begin and supplying smooth surfaces for the movement of bones at a joint, such as the cartilage shown in Figure 8.

Figure 8: A micrograph of the structure of hyaline cartilage, the type of cartilage that is found in the fetal skeleton and at the ends of mature bones.
The bones of the body gradually form and harden throughout the remaining gestation period and for years after birth in a process called endochondrial ossification. However, not all parts of the fetal cartilage are replaced by bone, cartilage remains in many places in the body including the joints, the rib cage, the ear, the tip of the nose, the bronchial tubes and the little discs between the vertebrae.
Endochondral Ossification
Endochondral ossification is the process of replacing cartilage with bony tissue, as shown in Figure 9. Most of the bones of the skeleton are formed in this way. During the third month after conception, blood vessels form and grow into the cartilage, and transport osteoblasts and stem cells into the interior which change the cartilage into bone tissue. The osteoblasts form a bone collar of compact bone around the central shaft (diaphysis) of the bone. Osteoclasts remove material from the center of the bone, and form the central cavity of the long bones. Ossification continues from the center of the bone toward the ends of the bones.

Figure 9: The process of endochondrial ossification which happens when the skeleton is developing during fetal development, and in childhood.
The cartilage at the ends of long bones (the epiphyses) continues to grow so the developing bone increases in length. Later, usually after birth, secondary ossification centers form in the epiphyses, as shown in Figure 9. Ossification in the epiphyses is similar to that in the center of the bone except that the spongy bone is kept instead of being broken down to form a cavity. When secondary ossification is complete, the cartilage is totally replaced by bone except in two areas. A region of cartilage remains over the surface of the epiphysis as articular cartilage and another area of cartilage remains inside the bone at either end. This area is called the epiphyseal plate or growth region.
When a bone develops from a fibrous membrane, the process is called intramembranous ossification. Intramembranous ossification usually happens in flat bones such as the cranial bones and the clavicles. During intramembranous ossification in the developing fetus, the future bones are first formed as connective tissue membranes. Osteoblasts migrate to the membranes and secrete osteoid, which becomes mineralized and forms bony matrix. When the osteoblasts are surrounded by matrix they are called osteocytes. Eventually, a bone collar of compact bone develops and marrow develops inside the bone.
Bone Elongation
An infant is born with zones of cartilage, called epiphyseal plates, shown in Figure 10, between segments of bone to allow further growth of the bone. When the child reaches skeletal maturity (between the ages of 18 and 25 years), all of the cartilage in the plate is replaced by bone, which stops further growth.

Figure 10: Location of the epiphyseal plate in an immature long bone. The chondrocytes in the epiphyseal plate are very metabolically active, as they constantly reproduce by mitosis. As the older chondrocytes move away from the plate they are replaced by osteoblasts that mineralize this new area, and the bone lengthens.
Bones grow in length at the epiphyseal plate by a process that is similar to endochondral ossification. The chondrocytes (cartilage cells) in the region of the epiphyseal plate grow by mitosis and push older chondrocytes down toward the bone shaft (diaphysis). Eventually these chondrocytes age and die. Osteoblasts move into this region and replace the chondrocytes with bone matrix. This process lengthens the bone and continues throughout childhood and the adolescent years until the cartilage growth slows down and finally stops. When cartilage growth stops, usually in the early twenties, the epiphyseal plate completely ossifies so that only a thin epiphyseal line remains and the bones can no longer grow in length. Bone growth is under the influence of growth hormone from the anterior pituitary gland and sex hormones from the ovaries and testes.
Even though bones stop growing in length in early adulthood, they can continue to increase in thickness or diameter throughout life in response to stress from increased muscle activity or to weight-bearing exercise.
Joints
A joint (also called an articulation), is a point at which two or more bones make contact. They are constructed to allow movement and provide mechanical support for the body. Joints are a type of lever, which is a rigid object that is used to increase the mechanical force that can be applied to another object. This reduces the amount of energy that need to be spent in moving the body around. The articular surfaces of bones, which are the surfaces that meet at joints, are covered with a smooth layer of articular cartilage.
There are three types of joints: immovable, partly movable, and synovial.
• Immovable Joint: At an immovable joint (or a fixed joint), bones are connected by dense connective tissue, which is usually collagen. Immovable joints, like those connecting the cranial bones, have edges that tightly interlock, and do not allow movement. The connective tissue at immovable joints serves to absorb shock that might otherwise break the bone.
• *Partly Movable Joints: At partly movable joints (or cartilaginous joints), bones are connected entirely by cartilage. Cartilaginous joints allow more movement between bones than a fibrous joint does, but much less than the highly mobile synovial joint. Examples of partly-movable joint include the ribs, the sternum and the vertebrae, shown in Figure 11. Partly-movable joints also form the growth regions of immature long bones.

Figure 11: Illustration of an synovial disk, a cartilaginous joint. These partly-movable joints are found between the vertebrae. An X ray of the cervical (neck) vertebrae is at right.
• Synovial joints: Synovial joints, also known as movable joints, are the most mobile joints of all. They are also the most common type of joint in the body. Synovial joints contain a space between the bones of the joint (the articulating bones), which is filled with synovial fluid. Synovial fluid is a thick, stringy fluid that has the consistency of egg albumin. The word ”synovial” comes from the Latin word for ”egg”. The fluid reduces friction between the articular cartilage and other tissues in joints and lubricates and cushions them during movement. There are many different types of synovial joints, and many different examples. A synovial joint is shown in Figure 12.
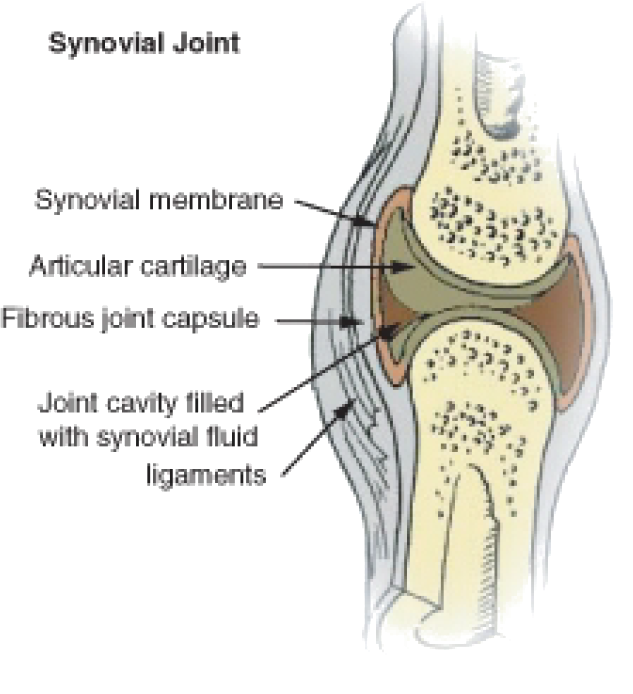
Figure 12: Diagram of a synovial joint. Sinovial joints are the most common type of joint in the body, and allow a wide range of motions. Think of how difficult walking would be if your knees and hips were only partly movable, like your spine.
The outer surface of the synovial joint contains ligaments that strengthen joints and holds bones in position. The inner surface (the synovial membrane) has cells producing synovial fluid that lubricates the joint and prevents the two cartilage caps on the bones from rubbing together. Some joints also have tendons which are bands of connective tissue that link muscles to bones. Bursae are small sacs filled with synovial fluid that reduce friction in the joint. The knee joint contains 13 bursae. Synovial joints can be classified by the degree of mobility they allow, as shown in Figure 13.

Figure 13: Types of Synovial joints. These fully-movable joints between bones allow a wide range of motions by the body. They also help reduce the amount of energy that needs to move the body.
In a ball and socket joint the ball-shaped surface of one bone fits into the cuplike depression of another. The ball-and-socket joint consists of one bone that is rounded and that fits within a cuplike bone. Examples of a ball and socket joint include the hip (Figure 15) and shoulder.
In an ellipsoidal joint an ovoid articular surface, fits into an elliptical cavity in such a way as to permit of some back and forth movement, but not side-to-side motion. The wrist-joint and knee (Figure 14), are examples of this type of joint.
In a saddle joint the opposing bone surfaces are fit together like a person sitting in a saddle. The movements at a saddle joint are the same as in an ellipsoid joint. The best example of this form is the joint between the carpals and metacarpals of the thumb.

Figure 14: Knee joint, an ellipsoid joint.

Figure 15: The hip joint is a ball-and-socket joint.
In the hinge joint, the articular surfaces fit together in such a way as to permit motion only in one plane, forward and backward, the extent of motion at the same time being considerable. An example of a hinge joint is the elbow.
The pivot joint is formed by a process that rotates within a ring, the ring being formed partly of bone, and partly of ligament. An example of a pivot joint is the joint between the radius and ulna that allows you to turn the palm of your hand up and down.
A gliding joint, also known as a plane joint, is a joint which allows one bone to slide over another, such as between the carpels of the fingers. Gliding joints are also found in your wrists and ankles.
Not all bones are interconnected directly: There are 6 bones in the middle ear called the ossicles (three on each side) that articulate only with each other. The hyoid bone which is located in the neck and serves as the point of attachment for the tongue, does not articulate with any other bones in the body, being supported by muscles and ligaments. The longest and heaviest bone in the body is the femur and the smallest is the stapes bone in the middle ear. In an adult, the skeleton makes up around 20% of the total body weight.
Homeostatic Imbalances of Bone
Despite their great strength, bones can fracture, or break. Fractures can occur at different places on a bone, and are usually due to excessive bending stress on the bone. Fractures can be complete in which the bone is completely broken, or incomplete in which the bone is cracked or chipped, but not broken all the way, as shown in Figure 16. Immediately after a fracture, blood vessels that were torn leak blood into surrounding tissues and a mass of clotted blood, called a hematoma, forms. The area becomes swollen and sore. Within a few days capillaries begin to grow into the hematoma and white blood cells clean up the dead and dying cells. Fibroblasts and osteoblasts arrive and begin to rebuild the bone. Fibroblasts produce collagen fibers which span the area of the break and connect the ends of the broken bone together. Osteoblasts begin to form spongy bone, and chondroblasts form cartilage matrix. Later, the cartilage and spongy bone are replaced by a bony growth called a callus which forms about 3 to 4 weeks after the fracture, and continues until the break is firmly sealed 2 to 3 months later. Eventually the bony callus is replaced by spongy and compact bone, similar to the rest of the bone.

Figure 16: Cracked collarbone.
Rickets is a softening of the bones in children which potentially leads to fractures and deformity; bowing of the leg bones is shown in Figure 17. Rickets is among the most frequent childhood diseases in many developing countries. The most common cause is a vitamin D deficiency. Vitamin D is needed by the body to absorb calcium from foods and to form bones. However, lack of calcium in the diet may also cause rickets. Although it can occur in adults, most cases of rickets occur in children who suffer from severe malnutrition, which usually results from starvation during early childhood. Osteomalacia is the term used to describe a similar condition occurring in adults, generally due to a deficiency of vitamin D. Osteomalacia can result in bone pain, difficulty in putting weight on bones, and sometimes fractures.

Figure 17: An X ray image of a 2-year-old who shows the typical bowing of the femurs that occurs in rickets. Rickets causes poor bone mineralization, which results in the bones bending under the weight of the body.
Some studies show most people get enough Vitamin D through their food and exposure to ultraviolet (UV) radiation in sunlight. Vitamin D is produced by certain skin cells from a compound found inside the cells. The skin cells need UV light for this reaction to happen.
However, eating foods to which vitamin D has been added or taking a dietary supplement pill is usually preferred to UV exposure, due to the increased risk of sun burn and skin cancer. Many countries have fortified certain foods such as milk, bread, and breakfast cereals with Vitamin D to help prevent deficiency.
Osteoporosis is a disease in which the breakdown of bone matrix by osteoclasts is greater than the building of bone matrix by osteoblasts. This results in bone mass that is greatly decreased, causing bones to become lighter and more porous. Bones are then more prone to breakage, especially the vertebrae and femurs. Compression fractures of the vertebrae and hip breaks, in which the top (or head) of the femur breaks are common, and can lead to further immobility, making the disease worse. Osteoporosis mostly occurs in older women and is linked to the decrease in production of sex hormones. However, poor nutrition, especially diets that are low in calcium and vitamin D, increase the risk of osteoporosis in later life. One of the easiest ways to prevent osteoporosis is to eat a healthful diet that has adequate calcium and vitamin D.
Osteoarthritis is a condition in which wearing and breakdown of the cartilage that covers the ends of the bones leads to pain and stiffness in the joint. Decreased movement of the joint because of the pain may lead to muscles that are attached to the joint to become weaker, and ligaments may become looser. Osteoarthritis is the most common form of arthritis. Some of the most common causes include old age, sport injuries to the joint, bone fractures, and overweight and obesity. Total hip replacement is a common treatment for osteoarthritis. An X ray image of a replacement hip joint is shown in Figure 18.

Figure 18: Total replacement of hip joint. One of the leading reasons for hip replacement is osteoarthritis of the joint in which the cartilage around the top of the femur bone deteriorates over time, and causes the bones of the joint to grind painfully against each other. This can result in a narrowing of the space in the ball-and-socket joint structure, causing limited movement of the hip and constant pain in the hip joint.
Images courtesy of:
http://www.flickr.com/photos/acaben/516493964/. CC-BY-SA.
Mariana Ruiz Villarreal. http://commons.wikimedia.org/wiki/File:Human_skeleton_front_en.svg. Public Domain.
Telethon. http://www.flickr.com/photos/ryanjunell/290767026/. CC-BY-SA.
http://training.seer.cancer.gov/anatomy/skeletal/classification.html. Public Domain.
http://training.seer.cancer.gov/anatomy/skeletal/tissue.html. Public Domain.
http://commons.wikimedia.org/wiki/Image:Compact_bone_-_decalcified_cross_section.jpg. GNU-FDL.
http://upload.wikimedia.org/wikipedia/commons/0/0f/Hyaline_cartilage.jpg. GNU-FDL.
USFG. http://training.seer.cancer.gov/anatomy/skeletal/growth.html. Public Domain.
USFG. http://training.seer.cancer.gov/anatomy/skeletal/growth.html ]. Public Domain.
http://www.flickr.com/photos/ciscel/382453477/. Public Domain, CC-BY-SA.
http://en.wikipedia.org/wiki/Image:Gelenke_Zeichnung01.jpg. GNU-FDL.
http://en.wikipedia.org/wiki/Image:Illu_synovial_joint.jpg. Public Domain.
http://www.flickr.com/photos/mexican/113765165/. CC-BY-SA.
Michael L. Richardson, M.D.. http://commons.wikimedia.org/wiki/Image:XrayRicketsLegssmall.jpg. CC-BY-SA 1.0.
Scuba-limp. http://commons.wikimedia.org/wiki/Image:Hueftgelenk-Endoprothese.jpg. GFDL 1.2, CC-BY-SA 2.5, 2.0, and 1.0.
http://en.wikipedia.org/wiki/Image:Illu_synovial_joint.jpg. Public Domain.